Injections for hernia lumbar spine - effective remedy to eliminate symptomatic pain caused by damage to the nerve endings of the vertebrae.
Hernia treatment with injections
Intervertebral hernia is a common disease that is characterized by a rupture of the fibrous ring, due to which an insignificant part of the nucleus pulposus falls out. The process is accompanied by infringement of the nerve base, passing near the place of prolapse, which leads to back pain.
When the condition is neglected, the patient is sent for a surgical operation. But its implementation is not mandatory. If the pathology is detected at an early stage, in order to eliminate pain and treatment, injections are used in the spine and other areas of the body located closest to the sore spot. They are more effective than painkillers in other dosage forms, because they are able to quickly deliver the substance to the problem area.
With the appearance of characteristic sharp pains in the back, you should immediately seek medical help. Pain medications such as ibuprofen, diclofenac, meloxicam and others of similar action are prescribed for temporary relief of pain. When administered, care must be taken not to exceed the permitted daily dose.
Steroids are also used for pain relief. These include betamethasone, prednisolone, methylprednisolone, which are injected directly into the affected intervertebral nerve.
On the initial stage hernia development are sometimes assigned intravenous injections medicines with a dropper. For this purpose are used:
- analgesics, which include paracetamol and aspirin for pain relief;
- vinpocetine to improve blood circulation and prevent congestion;
- eufillin for oppression inflammatory process and anesthesia;
- actovegin for the relief of pain in the nerve endings.
 When a hernia occurs, the muscle fibers of the back become tense and cannot return to a relaxed state on their own. To eliminate spasm muscular system injections with muscle relaxants are prescribed. Since they are fast-acting drugs, relief after their use comes very soon.
When a hernia occurs, the muscle fibers of the back become tense and cannot return to a relaxed state on their own. To eliminate spasm muscular system injections with muscle relaxants are prescribed. Since they are fast-acting drugs, relief after their use comes very soon.
To prevent the development of the disease, injections with chondroprotectors are used, which contribute to the nutrition of the cartilage tissue of the vertebrae. They are part of medicines:
- don;
- structum;
- alflutop.
Substances of this group differ characteristic feature: They have a long absorption time. Therefore, for effective action the course of injections is up to six months. Reception goes according to the scheme drawn up by the attending physician.
Blockade for hernia treatment
Injections for a hernia of the spine are divided into two varieties:
- Intercostal injections of novocaine. The essence of the procedure is to inject the medicine into the place of infringement of the nerve ending. According to the injection site, the procedure is divided into posterior, lateral, anterior and parasternal.
- epidural blockade. The principle of operation of the procedure is the introduction of an anesthetic into the epidural space of the vertebral canal. It is located between solid meninges and the periosteum of the canal, which connect special strands. During the injection, the medicine enters the sore spot due to the fact that they are separated. With repeated injections, the penetration of novocaine is easier and more efficient.
- Mixed blockade is carried out by simultaneously administering antihistamines and anti-inflammatory drugs. It is used only if the previous methods did not bring positive results.
Before injections from a hernia of the spine are prescribed auxiliary procedures aimed at determining the location of the pinch (ultrasound, computed tomography).
Injections are carried out only by an experienced specialist. He must feel the sacral horns, which are located a little further from the desired spinal canal, and inject the drug.
 Blockades are carried out with the help of anesthetics, lidocaine or novocaine is used. Due to their high efficiency, they are able to eliminate pain syndromes in the shortest possible time. The effect of painkillers lasts up to three weeks, but they cannot be administered more than once a week.
Blockades are carried out with the help of anesthetics, lidocaine or novocaine is used. Due to their high efficiency, they are able to eliminate pain syndromes in the shortest possible time. The effect of painkillers lasts up to three weeks, but they cannot be administered more than once a week.
In the presence of severe inflammation, blockade injections with corticosteroid preparations are prescribed. They are characterized by high efficiency and easy digestibility. These include:
- celeston;
- dexamethasone;
- cortisol;
- lorinden.
Injection blockades have minimal adverse reactions, therefore they are placed in patients of any age and category.
Features of the epidural blockade
For the correct implementation of the epidural blockade, the patient lies on his side, bending his legs towards the stomach. Anesthesia can be carried out either through the introduction of drugs with a dropper, or by creating a "lemon peel", when the anesthetic is injected directly at the site of the operation under the skin.
The procedure is performed in accordance with the following steps:
- The anus of the patient is isolated with tampons and towels.
- Processing in progress skin disinfectant, during which the specialist gropes for the vertebrae and the place for inserting the needle.
- The injections are made with a six-centimeter needle, introducing it with a sharp movement to quickly reach the sacral canal.
- There is a sharp change in the direction of the needle in the opposite direction. To get the desired effect, it must be inserted five centimeters and lowered down.
- The location of the needle is checked by opening the plunger of the syringe. If the procedure is carried out correctly, foreign fluids (blood, cerebrospinal substance) should not appear in it.
- After making sure that the location is correct, the medicine is injected very slowly and smoothly.
- After the procedure is completed, the patient remains in the original position for at least 30 minutes.
The procedure for conducting an epidural blockade requires certain skills and knowledge. In order not to harm motor apparatus wrong actions, it is strictly forbidden to do it yourself.
To provide medical care at intervertebral hernia injections are given. What injections are given? In the initial stages of the disease, steroid and non-steroidal drugs, chondroprotectors and muscle relaxants are used for injections. But with severe pain, only lidocaine or novocaine blockades can help. Whatever drugs are used, to cure the disease, you must follow the doctor's instructions.
One of the main symptoms of a spinal hernia is severe pain. That is why painkillers for hernia of the spine is a mandatory drug used at the initial stage of treatment of this pathology. Taking drugs in any pharmacological form that have an analgesic effect allows you to solve several problems at once in the form of eliminating obvious discomfort, partially relieving the inflammatory process, as well as normalizing the general mental state of the patient.
How a hernia of the spine hurts depends on the stage of development of the pathology. At the same time, in the absence of treatment, not only the nature of the pain and its intensity change, but also the place of manifestation of this symptom.
On the early stages diseases, pain manifestations are aching in nature. The pain itself is dull. Its strengthening occurs with a long stay in a sitting position, as well as when lifting various weights. Significant relief at this stage occurs when taking a horizontal position of the body.
In the absence of proper treatment, there is an intensive growth of the hernia, and a change in the nature of the pain. It becomes aching and shooting, and its localization expands significantly. Depending on the location of the hernia, pain can radiate to the leg, back of the head, under the shoulder blade. Gradual damage to nerve endings provokes pain even in the heel, thumbs or on the back of the feet. While coughing or sneezing pain are greatly amplified. Some relief comes from the adoption of a horizontal position of the body, while it is necessary to lie on a healthy side, slightly bending the legs at the knees.
The main groups of painkillers
Pain associated with spinal hernia can be treated with a variety of medical devices. All of them can have different shape release. These are tablets, solutions for intramuscular injections, ointments and gels. Most often, injections are used for effective and quick pain relief. At the same time, ointments and gels have the least number of contraindications. But they are not as good at relieving pain as injections or pills. And with the wrong selection of a drug or its incorrect use, it quite often provokes the development of skin reactions in the form of a rash.
Based on its composition, an anesthetic drug used in the treatment of spinal hernia may belong to one of the following groups of medicines:
- non-steroidal anti-inflammatory drugs;
- painkillers that do not contain narcotic substances;
- narcotic analgesics;
- muscle relaxants;
- hormonal medicines.
In a certain dosage, the preparations of each of these groups of drugs can relieve pain symptoms.
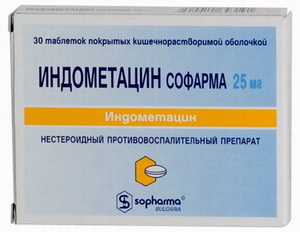
Non-steroidal anti-inflammatory drugs
 An anesthetic for hernia of the spine, belonging to this group of drugs, allows not only to effectively and quickly relieve pain, but also helps to relieve the inflammatory process and eliminate puffiness. The most effective drugs in this group include:
An anesthetic for hernia of the spine, belonging to this group of drugs, allows not only to effectively and quickly relieve pain, but also helps to relieve the inflammatory process and eliminate puffiness. The most effective drugs in this group include:
- Diclofenac;
- Indomethacin;
- Ketoprofen;
- Amidopyrine.
And although these drugs allow you to quickly and efficiently anesthetize the patient with a vertebral hernia, however, their long-term use is prohibited. The reason for this lies in the very strong effect of this type of drug on work. gastrointestinal tract as well as the liver.
Pain medications that do not contain drugs
 The answer to the common question about what to do if the patient cannot continue taking nonsteroidal drugs, most often is the appointment of painkillers, which do not contain narcotic components. The most effective of them include:
The answer to the common question about what to do if the patient cannot continue taking nonsteroidal drugs, most often is the appointment of painkillers, which do not contain narcotic components. The most effective of them include:
 “Complete healing of joints and back for 1 RUBLE!”
“Complete healing of joints and back for 1 RUBLE!”
A federal program has been launched to rid the population of diseases of the musculoskeletal system! It's hard to believe but effective drug funded by the Ministry of Health. Terrible statistics show that a banal crunch and pain in the joints often end in disability! To avoid this, you need to take a penny remedy ...
- Dicloberl;
 Removal of pain from a hernia of the spine with the help of such drugs occurs due to the partial blocking of the components of these drugs, individual areas of the brain responsible for the analysis and perception of pain.
Removal of pain from a hernia of the spine with the help of such drugs occurs due to the partial blocking of the components of these drugs, individual areas of the brain responsible for the analysis and perception of pain.
Many patients, in order to conduct anesthesia for a hernia of the spine, take only Analgin. However, such an action is very dangerous, since this drug, which partially relieves pain, has a serious toxic effect on the kidneys and circulatory system. Very quickly, the pain with the help of Analgin will practically cease to be removed, and pathological condition quickly supplemented by destructive conditions in vital organs and systems.
Narcotic type analgesics
The use of drugs in this group is possible only after their direct appointment by the attending physician. The intake of such drugs occurs when a herniated disc is accompanied by extremely strong, unbearable pain. However, due to the extremely strong action, you can use such medicines for an extremely short period of time.
The most effective narcotic-type analgesics include drugs: Tramadol, Morphine, Codeine and Fentatin. Their impact on the hernia occurs indirectly. The process of pain relief is carried out due to the complete relaxation of all muscle groups as a result of the direct influence of the components of the drug on the brain. Such drugs contribute to such a phenomenon as narcotic sleep.
Muscle relaxants
 Muscle relaxants can effectively reduce and eliminate the manifestations of pain in spinal hernia. These drugs are conditionally divided into 2 groups:
Muscle relaxants can effectively reduce and eliminate the manifestations of pain in spinal hernia. These drugs are conditionally divided into 2 groups:
- central action;
- peripheral action.
When using centrally acting muscle relaxants, the damaged area of the body stops hurting due to the effect of the main components of the drug directly on the parts of the brain responsible for the reaction to pain. They also affect the functioning of the central nervous system.
 Peripheral-type drugs affect only the nerve endings, thus contributing to the complete relaxation of tense areas of muscle tissue.
Peripheral-type drugs affect only the nerve endings, thus contributing to the complete relaxation of tense areas of muscle tissue.
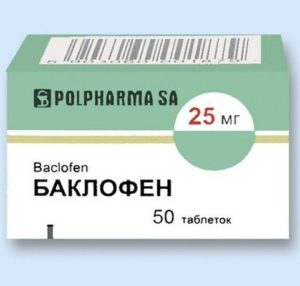
To the most popular drugs from the group of muscle relaxants, in the treatment intervertebral hernia, include the drugs Sirdalud, Baclofen, Tizanidin, Methocarbamol, Orphenadrine, Mydocalm and Clonazepam.
Hormonal drugs
In order to save a vertebra damaged by a hernia and other parts of the body from extremely severe pain, hormonal drugs can be used in emergency cases. They are very effective in fighting pain and inflammation. However, for safe use hormonal drugs, strict adherence to all prescriptions regarding dosages and regimens is necessary. AT otherwise high risk of complex side effects hormonal background and the immune system.
In some cases, special hormonal preparations are used for treatment, the introduction of which to the patient is possible only in special protected rooms and in overalls, to protect against aggressive healthy person components.
Dexamethasone is one of the most used analgesic type drugs used for spinal hernia.
All drugs with an analgesic effect used to anesthetize a vertebral hernia are potent. Their incorrect selection, as well as use, easily provoke the occurrence of serious side effects. That is why, for safe and effective treatment vertebral hernia with the use of painkillers, it is necessary to consult your doctor.
Do you still think that getting rid of osteochondrosis is not easy?
Have you tried all possible means, but the pain does not recede and prevents you from living a full life? Apparently yes, since you are reading these lines, and not playing with your children and grandchildren.
Stop adapting to back and joint pain, we strongly recommend reading Dr. Dikul's article on how to get rid of osteochondrosis and back pain...
With a lumbar hernia, the nerve roots are affected. Infringement of the nerves is accompanied by severe pain, inflammation, impaired blood flow. Doctors prescribe injections for a hernia of the lumbar spine, with their help they stop pain, suppress inflammation, and establish the transport of nutrients to the lesion.
Choice of drugs
After examining the patient, the doctor decides which injections will effectively relieve pain, swelling and inflammation, and at the same time will not give adverse reactions, which are possible with concomitant pathologies.
The course of the disease affects the method of administering drugs - intramuscularly or intravenously. In mild forms, injections are made intramuscularly. In severe cases, intravenous injections are given.
Vertebral hernia is treated:
- nonsteroidal drugs (NSAIDs);
- analgesics;
- steroid medicines;
- muscle relaxants;
- chondroprotectors;
- diuretic drugs;
- group B vitamins.
The action of non-steroidal anti-inflammatory drugs
Injections of non-steroidal drugs anesthetize, suppress the inflammatory process, relieve swelling and temperature. Such injections are given intramuscularly.
Usually between vertebral hernias appoint:
- Indomethacin;
- ibuprofen;
- Diclofenac.
The impact of analgesics
Intramuscular injections with analgesics quickly relieve pain. At the same time, the analgesic effect provided by them is short-term. They do not affect the causes of the disease and do not eliminate them. Medicines are used when there are no potent drugs.
For pain relief use:
- Analgin;
- Baralgin.
The effectiveness of steroids
An injection of steroids reduces inflammation and eliminates pain. The drugs are injected directly into the damaged nerve ending. After an intramuscular injection, patients do not feel pain for a year.
Steroids cannot cure any spinal hernia. Hernial protrusions are eliminated with the help of therapeutic gymnastics or operationally.
To relieve pain and inflammation, injections are prescribed:
- Betamethasone;
- Prednisolone;
- Triamcinolone;
- Methyl Prednisolone.
Action of muscle relaxants
A herniated disc causes tension in the back muscles. Tight muscles help support the skeleton. Tension leads to muscle spasms. To relieve spasms and relax muscles, the doctor prescribes muscle relaxants:
- Mydocalm;
- Ditilin;
- Tizanidine;
- Sirdalud;
- Baclofen;
- Metaxalon.
The introduction of these drugs prevents further disc shift. Muscle relaxants are fast-acting drugs. The patient feels relief after the first injection.
The drugs have serious side effects. They provoke the appearance of mental disorders. An overdose of them is a threat to life.
The influence of chondroprotectors
The progression of the disease is stopped with the help of chondroprotectors. Patients for tissue repair are often prescribed:
- Don;
- Rumalon;
- Hondrolon;
- Elbon.
Chondroprotectors nourish cartilage tissues, promote their regeneration. They provide lubrication to the joints. Thanks to them, the process of destruction of cartilage structures is suspended. The cartilage matrix becomes elastic again. Since drugs from this category are slowly absorbed, they are treated for quite a long time (up to 6 months).
Effect of diuretics
The use of diuretics speeds up recovery. They relieve swelling, which helps to reduce pain. Patients are prescribed injections:
- Lasix;
- Furosemide.
B vitamins
Vitamins in injections, strengthening the body's resistance, help fight intervertebral hernia. With lumbar hernia, injections are made:
- Milgamma;
- Vitakson.
blockades
Patients with severe forms experience unbearable pain. They remove the strongest pain syndrome by making blockades. For pain relief, more often than other anesthetics are used:
- Novocaine;
Blockades with them quickly suppress pain at the site of the formation of a hernial protrusion. 
At severe inflammation Patients are given blockades with corticosteroids. Cope with the elimination of symptoms:
- Celeston;
- Flucinar;
- Cortisol.
When other methods fail positive result, appoint mixed blockades. For their implementation, drugs with antihistamine and anti-inflammatory action are used.
Performing a blockade, the doctor makes an injection directly into the spine, where the hernial protrusion has formed. The drug penetrates into the damaged nerve fibers, due to which the pain recedes.
Novocaine blockade
Unbearable pain occurs due to the fact that the shifted intervertebral disc pinches the nerve roots. A large hernia blocks the blood flow with which medicines enter the lesion. Because the active substances do not reach the damaged nerve roots, the pain syndrome does not disappear.
If the injections do not stop the pain, novocaine or lidocaine blockade is done. The solution injected into the pinched nerve ending quickly suppresses the pain syndrome.
The blockade is performed by a doctor who knows how the nerve roots are located. To exclude medical errors before the procedure, the patient undergoes hardware studies: ultrasound or computed tomography. The pictures clearly show the location of the hernia. Thanks to them, the doctor accurately injects the painkiller.
Blockades - effective method anesthesia. The action of one injection is enough for 7 days.
epidural blockade
The blockade is performed using novocaine and a steroid agent. Medicines enhance the analgesic effect of each other. This combination of drugs quickly copes with the suppression of pain. The injection is given between the periosteum and the spinal canal. The retracted connecting cords allow the solution to penetrate into the affected area.
Such injections for a hernia of the spine are done by a doctor. He injects an analgesic solution into the sacral canal using a 6 cm needle. During the blockade, the patient is in the fetal position. The blockade is valid for 14-48 days.
Droppers
In the early stages of the disease, droppers are prescribed. With their help, medicinal solutions are administered intravenously. Active substances immediately enter the bloodstream and are transported to the lesion.
 To relieve pain, a solution of aspirin or paracetamol is administered intravenously. Vinpocetine droppers normalize blood flow, eliminate congestion in the lesion.
To relieve pain, a solution of aspirin or paracetamol is administered intravenously. Vinpocetine droppers normalize blood flow, eliminate congestion in the lesion.
The site is a medical portal for online consultations of pediatric and adult doctors of all specialties. You can ask a question about "injections for a hernia of the lumbar spine" and get free online consultation doctor.
Ask your question Ask your questionQuestions and answers on: injections for a hernia of the lumbar spine
2016-03-29 11:14:57
Alena asks:
Hello, now I am treating a hernia of the cervical and lumbar spine, they put me on a dropper, give me 5 injections and take pills. And today they made a blockade in a place where there is very strong pain. Tell me, please, do I need to take something for the stomach, liver and kidneys with so many drugs?
Responsible Vasquez Estuardo Eduardovich:
Good afternoon, Alena! It would be wrong to interfere with the treatment that is being carried out by other doctors. Ask your questions to your doctor.
2015-06-30 06:24:55
Sergei asks:
Lumbar lordosis saved.
Thanks for the early.
Responsible Starish Natalya Petrovna:
Hello! It is unrealistic to remove protrusions, hernias and your osteophytes with medication. This is a physical problem that is solved with the help of physical factors - physiotherapy (magnet, laser, myostimulation, shock wave therapy, ultrasound, massages, vacuum therapy). It makes sense to buy and wear a rigid lumbosacral corset when moving in transport and physical. load, but not more than 2-3 hours a day. It is necessary to dress it only lying down, in a relaxed state. It makes sense to do static exercises aimed at strengthening the muscular-ligamentous corset. Eliminate heavy lifting, leaning forward and a long stay in the "sitting" position. Manual therapy is contraindicated.
2015-06-26 12:30:44
Sergei asks:
Good time of the day. Tell me what to do, I did an MRI a year ago In conclusion:
Lumbar lordosis is preserved.
A moderate decrease in height is determined while maintaining the intensity of the signal in the intervertebral discs L4-5 L5-S1; small posterior osteophytes of the vertebral bodies.
"Small" cartilaginous nodes of the vertebral bodies.
Protrusion of the intervertebral disc L4-5 (poster-central) up to 3.3 mm in size, with slight compression of the dural sac.
The subarachnoid space is free, compressed at the level of protrusion.
Conclusion: MRI signs of chondrosis intervertebral discs L4-5 L5-S1; spondylosis of the lumbar spine, protrusion of the intervertebral disc L4-5.
My back hurt from time to time. Lately, almost all the time. Almost immediately after the MRI I pierced "ALFLUTOP" 20 pcs. then I found a twisting exercise on the Internet, where a person describes how he was treated for a hernia. http://ovuk.ru/ What would you advise to pierce and what to do to get rid of a hernia?
I do the exercise, it helps, the pain goes away, but not for long.
I want to pierce a series of injections described http://ovuk.ru/vazhnaya-informaciya.html. What do you say and advise.
Thanks for the early.
Responsible Starish Natalya Petrovna:
It is unlikely that you will be able to completely remove the hernia. It can be reduced. When it decreases, it will release the nerve root and the pain will go away on its own. To do this, you need to undergo a course of competent physiotherapy, apply chondroprotectors and engage in exercise therapy. In the future, it is necessary to exclude hypothermia, heavy lifting and stress.
2013-12-17 19:04:05
Julia asks:
Hello! Help deal with the situation. MRI examination of the lumbar spine was performed in the sagittal and axial projections in T1 and T2 WI. The height of the vertebral bodies is not changed. The endplates of the L1-L3 vertebral bodies are deformed by Schmorl's hernias. Subchondral reaction of L4-L5 vertebral bodies. The height of m / n disks in the L4-S1 segment is reduced, the intensity of the MR signal in T2VI is reduced due to dehydration of the pulpous nuclei of the disks. Dorsal protrusions of m/n discs are visualized: - L5-S1 - 0.4 cm - median variant, s/m channel - 1.1*1.3 cm; - L4-L5 - 0.45 cm - wide median version, s / m channel - 1.0 * 1.7 cm. Cone spinal cord and ponytail without features. Conclusion: Signs of osteochondrosis of the lumbar spine. Mri was done on 08/14/13. I am 23 years old. Height 169 cm, weight 52 kg. Say these are large protrusions, far from hernias, the word median dorsal protrusion is very frightening. What is the wide median? I am very afraid of lumbago, because I endured two of them, but such that now it’s just a phobia! The first one was a year ago before the MRI, the 2nd in September, she was treated with injections, ointments, then physical procedures. 2. A month ago I was treated in a balneological hospital, where I underwent underwater traction of the spine, paraffin therapy, acupuncture, massage, electro-procedures, radon baths, a bioregulator, a bioptron. Now I do it almost every day. physiotherapy exercises which was done in the hospital. But the problem is that the pain is still there, sometimes less then more, and this has been going on for a year. When walking, they quickly get tired and the muscles of the lower back begin to hurt, constant feeling stiffness in the region of the sacrum. Sometimes when walking, the feeling that the legs are wadded. They brought me an inversion table, hung on it at an angle of 30 degrees, but after a couple of days the pain in my lower back intensified. I don’t work now, I lie down a lot, I try to sit at the computer as little as possible, I don’t want to burden the spine. Is lying good for protrusions or is it better to move more? Tell me whether it is possible to cure protrusions at all or is it for life and you need to maintain a physical condition so that it doesn’t get worse. Am I eligible for conservative treatment? How bad are dorsal median protrusions?
Responsible Zolotoverh Alexander Mikhailovich:
Dear Julia,
Judging by the MRI descriptions you sent, there are no indications for surgery. Answering your questions, I would like to note that it is better to go into the details of the MRI description less, since the content of the description of the MRI picture is intended purely for a specialist.
Definitely, with degenerative diseases of the spine, it is better to move more and maintain your physical condition. Conservative therapy must be carried out during an exacerbation or 1-2 times a year, sanatorium-and-spa treatment is also indicated.
2013-04-07 15:09:28
Peter asks:
Hello. My name is Peter, I'm 42 years old, 7 years ago an intervertebral hernia was removed, it was 11 mm. According to the results of the MRI, there was another hernia (I don’t remember how many millimeters), it was not removed. After the operation, everything was fine, but a month ago my right leg started to hurt. Two weeks ago I went to the hospital, but I didn’t feel better, I move only with crutches, severe pain in the leg. Did a new MRI. Please explain to me what everything that is written there means, how many millimeters I have a hernia and what needs to be done with such an MRI conclusion, I am attaching the conclusion.
The resulting images show a decrease in the height of the L3-S1 intervertebral discs, a decrease in the MR signal from their structures on T2 images. On the adjacent surfaces of the lumbar vertebrae, bone growths - osteophytes are determined. The sagittal size of the spinal canal at the studied level is 12.4 mm.
At the L5-S1 level, the intervertebral disc is displaced by 7.5 mm into the spinal canal paramedianly and intraforaminal to the right with sequestration?, compresses the dural sac and its contents, the right intervertebral foramen, and compresses the S1 roots on the right.
The intervertebral disc L4-L5 will stand in the spinal canal paramedian to the right up to 3.87 mm, compressing the right intervertebral foramen, roots L5.
The narrowing of the intervertebral foramens, the spinal canal is determined due to hypertrophy of the yellow ligaments and facets of the intervertebral joints.
The spinal cord is not changed, its contours are clear, even, the structure is homogeneous. Lumbar lordosis is smoothed. Paravertebral soft tissues without features. Bone-destructive changes were not revealed.
Are determined degenerative changes on adjacent surfaces of L5S1 vertebrae.
CONCLUSION: MRI picture of osteochondrosis of the lumbar spine, arthrosis of the facet joints.
Herniated discs L5S1, L4L5.
I went through a course of treatment with Voltoren (injections) and made three injections of Artoxan. tell me what injections are stronger you can still take? Thank you!
Answers:
Hello Peter. You have progressive osteochondrosis, like most people. Neurosurgeons, of course, will suggest surgery. If you have the desire and money, you can do it, but as you understand, this is a temporary measure and you cannot operate on all the disks. Treatment by a neurologist.
2011-03-28 21:11:58
Artem asks:
Good evening! I'm 28 years old. Had a CT scan of the lumbar spine.
The protrusion of the intervertebral discs L4-L5 up to 5 mm dorsally, L5-S1 up to 7 mm with lateralization to the left, pushing the dural sac and elements of the epidural space dorsally, and reducing the volume of the left lateral pocket are determined. Bone sharpening is noted in the anterolateral parts of the vertebral bodies at the level of L1-S1. In the body L2 Schmorl's hernia.
There is no particular pain, mostly sometimes a slight pain when bending over. I am very interested in the occupation of the little toe of the left foot along the foot to the heel on the side. It feels like poor blood circulation. And it's been like that for two months. I have been seeing a neuropathologist for about a month and a half. First, they gave anti-inflammatory injections, and also went to the treatment room (magnet, amplipulse). Now I am giving Mukosat injections.
What to do with the fact that the occupation of the little finger of the left leg along the foot to the heel on the side.
Responsible Korotruchko Anatoly Alexandrovich:
Hello Artem, numbness of the toe is a violation of sensitivity and is not caused by a violation of blood flow, but by pathological changes in your spine. If this bothers you a lot and your treatment is ineffective, come to us for a consultation and treatment. If it doesn't really bother you, you can wait, but you will have to deal with a pain center or neurosurgeons.
2011-02-10 15:45:20
Angela asks:
I am 40 years old, I live in Kirovograd, height is 168 cm, weight is 84. Osteochondrosis has been bothering me for almost 20 years, especially lumbosacral. Previously, the pain was given in left leg and buttock, now to the right.
I had an MRI on 12/01/2010. Description: On a series of MRI tomograms, the axis of the spine from the midline in the lumbar region is somewhat deviated to the left. Reduced height L4-L5, L5-S1 m / n disks; reduced intensity of the MR signal from them, on T2 VI, due to dehydration. In the adjacent subchondral areas of the bodies of L5, S1 vertebrae, there are areas of fatty degeneration. Circular protrusion L4 - L5 m / n disc, which protrudes into the spinal canal and m / n holes (mainly left) up to 3.7 mm. Ppotrusion L5 - S1 m / n disc, which protrudes into the spinal canal up to 2.0 mm. The back of the brain in the visible extent b / o. The anteroposterior size of the spinal canal at the level of L3 is 14.4 mm. Conclusion: Protrusion m / n discs. MR signs of osteochondrosis of the lumbar spine (at the level of L4 - S1). scoliotic curvature spinal column at the level under study. In words, they said that there is a hernia, but not yet such as to write in conclusion - be treated, growth may stop.
The neuropathologist prescribed treatment, went to work and was treated in parallel (from 02.12. to 23.12. injections, tablets - amplipulse and magnet procedures) it became worse. 24.12.2010. went to the hospital, they made 3 droppers with an anesthesia complex. For more than 30 minutes, the right leg could not walk, during this time from 3 to 5 times inward to the left leg. It was painful to walk, stand and naturally sleep at night. Pain of the type of convulsive, numbness of the foot appeared at first thumb by the end of the 3rd day, the floor of the foot became numb and still does not go away. 01/05/2011 was put in a hospital, lay for 15 days - every day a dropper, on 11.01 they did a CT scan
CT scan: L 3-4-circular protrusion MPD- 3 mm
L4-5 against the background of circular protrusion, dorsal medial hernia of mpd-6.8 mm, stenosis of the root canals.
L5-S1 dorsal protrusion of IVD 4mm, "vacuum phenomenon"
Conclusion: hernia L 4-5 mpd. Protrusions L3-4, 4-5-5-S1. Dystrophy of the nucleus pulposus L5-S1 mpd. Spondylarthrosis
The conclusion of the neurosurgeon:
Diagnosis: right-sided posterolateral hernia L4-L5 MPO with compression of the root L5. Persistent pronounced pain radicular syndrome on the right. Kyphoscoliosis II stage.
Recommended: surgical treatment. Discharged on 19.0111. to open sick leave. Diagnosis: Rozpovsyudzheny osteochondrosis of the ridge with major lesions of the cervical and transverse vertebrae of the III degree. Right posterior-lateral keel L4 -L5 mxd with compression of the core L5. Steady expressions of pain, brown with m. Kyphoscoliosis II stage. NPH II Art. PBMC II Art.
Treatments: dexalgin, no-shpa, dexazone, L-lysin, furosemide, asparkam, milgama, movalis, mildrocard, eglonil, lotren, airtal, midocalm, xefocam, triphas, tizanidine, declac gel. Written out from the vіddіlennya according to the completed lines of the statutory liquidation. Stan middle.st.importance. Bol'ovy s-m peace of expressions. Damaged function of walking. One is saved along the L5 course of the right. Recommended: Virishiti nutrition about operational excellence. Since 20.01 I have been sick at home, the numbness of the foot does not go away, convulsive pains are constantly pursuing right foot. When you touch the foot, the pain is as if the body is moving away from anesthesia (they break a finger or cut it alive). I walk with a stick for short distances around the house or in the clinic, after 5 minutes I get tired, my legs give way - I have to sit down to rest. Pain in the leg is constantly present, especially now in the ankle and the lower leg itself. Lying down, it is not possible to turn around from pain in the right buttock immediately accompanied by convulsive pain all over the leg. I try to do at least some kind of exercise for only 5 minutes, in a dream I wake up from pain after the body reflexively wants to pull up an arm or leg, sometimes even just movements heads. I'm afraid to do the operation, people were intimidated that the hernia resumes in a couple of years at the same place. Is conservative treatment possible? Where is it better to have an operation, how much money do you need to prepare? Is laser therapy possible?
Responsible Kachanova Victoria Gennadievna:
Hello Angela. You treated conservatively, took a fairly large complex of medications, but did not get any effect. It is better to do the operation in Kharkov, Kyiv or Donetsk. I don’t know about the financial side, everyone will say on the spot. Laser therapy is carried out in Kyiv. Whether it is possible in your case, only a specialist decides after consultation.
2011-01-21 00:28:51
Elena asks:
Hello Doctor! I would like to know your qualified opinion about my husband's disease. He is 52 years old. Spinal diseases have never been detected before.
Two weeks ago, mild pains appeared in the back, radiating to the left leg. We turned to a neuropathologist. They prescribed droppers and injections.
After treatment:
MRI dated 01/15/2011
The normal degree of lumbar lordosis is determined, without signs of segmental shortening.
The vertebral bodies have a normal configuration, relationship and trabecular structure.
Along the contour of the adjacent end plates L5, S1, zones of degenerative changes are noted.
Significantly pronounced osteophytes are determined along the anterior surface of the L5 S1 bodies.
Along the lower surface of L5 and along upper surface S1 marked uneven thinning and deformation of the cortical layer.
At the level of L3-L4, L4-L5, L5-S1, there is a decrease in the height of the intervertebral discs and a decrease in their intensity of the MR signal in T2-WI, due to dehydration.
At the L3-L4 level, a local protrusion of the disc is determined posteriorly and paramedially to the right up to 5.2 mm, towards the left intervertebral foramen up to 4 mm.
At the level of L4-L5, the protrusion of the disc towards the left intervertebral foramen up to 4 mm is determined.
At the level of L5-S1, the protrusion of the disc is determined posteriorly and paramedially to the left up to 3.4 mm, towards the left intervertebral foramen up to 4 mm.
The spinal canal has a normal sagittal size. No additional formations or areas of variable MR signal intensity were found in the spinal canal.
Pre- and paravertebral soft tissues without features.
Conclusions: MRI signs of osteochondrosis of the lumbosacral spine with predominant localization in the L5-S1 segment.
Protrusions of discs L4-L L5-S1. Herniated disc L3-L4. Spondylosis bodies L5, S1
Treatment takes the second week. 6 initial days of drip. Piracetam, magnesium sulfate, trental, mydocalm, neurorubin, dicloberl, carbamazepine.
Currently accepting:
Discus compositum, alflutop, mydocalm, neurorubin, neuromidin, arcoxia.
Ointment Zhivokost, Diclofenac, Chondroxide, Dolobene.
Throughout the entire time of the disease, he experiences severe pain, despite constant painkillers (dikloberl, ketanov, dexalgin). Most of the pain prevails in the left leg from the hip to the knee.
We received a consultation from a neurosurgeon, there was no talk of surgical treatment. He prescribed the treatment that we are taking today.
We use the Lyapko applicator.
They took a special orthopedic corset. They said to wear it all the time, only when you lie down - take it off!
Four times withstood the electric massage.
The pain is very severe. Permanent! From painkillers, they only become a little dull.
Maybe the treatment isn't enough?
What would you advise, wasn't the pain supposed to subside during 2 weeks of treatment?
Thank you for your attention and your time devoted to us!
We are looking forward to an answer.
Determined median posteriorly, hernia m/p disk L5-S1 with compression of the dural sac, dimensions: longitudinal 5 mm. height 10 mm, transverse 14 mm; against the background of protrusion forward paramedian to the left up to 9 mm, to the sides up to 4 mm. spinal canal longitudinal size up to 19 mm, width up to 17 mm C-shaped scoliosis 2 tbsp. deforming spondylosis and spondylarthrosis of the lumbosacral spine. At the moment, the back does not hurt, very worried nagging pain in the left leg, especially under load. I think that the pain in the leg is related to problems in the spine. Explain in what ways (medication, physical exercises, surgery to remove hernias) pain in the leg can be identified. Will Lyapko's applicator help? Thanks in advance for your advice and suggestions. Thank you.
Responsible Samonenko Yury Mikhailovich:
Hello. Judging by the description of the pictures and your complaints, most likely your pain is associated with compression of the nerve root in spinal canal herniated disc.
In order to put an indication for surgery for a herniated disc, you need:
1. Complaints of pain along the radicular nerve
2. The presence of a herniated disc on MRI or CT scan with signs of compression of the CORRESPONDING radicular nerve. (for example, a hernia at the level of L5-S1 cannot cause compression of the L4 radicular nerve, and another cause must be sought)
3. The duration of the disease is not less than 2-3 weeks and not more than 4-6 months in case of ineffective conservative treatment(in more early dates surgery is indicated if there are signs of prolapse motor function nerve or with unbearable pain).
4. The presence of tension symptoms from pain.
A fairly serious disease of the spine, which in everyday life is often referred to as "disc prolapse", and among physicians has a long name "herniated disc of the lumbar spine", often requires surgical operation. However, Japanese scientists have created a drug based on a special enzyme that some types of bacteria secrete in the process of life. A single injection into the affected area causes the strangulated tissue to dissolve, just as if it had been excised with a surgeon's scalpel.
Hernia - pathology, which develops gradually, can lead a person to disability in the absence of timely measures taken . Her treatment is not without the use of painkillers both at the stage of using medications and after surgery . Therapy of a vertebral hernia requires caution in taking drugs that reduce pain, since in addition to inhibiting pain, they can cause significant harm to the body. Therefore, self-administration of drugs for this disease is out of the question.
Painkillers for spinal hernia are prescribed by the attending doctor after an in-depth diagnosis of the state of the intervertebral disc and the degree of protrusion of its nucleus. It is important to note that the analgesic effect after taking the medication is temporary and after a while the procedure will have to be repeated. Periodic pain relief is not a direct treatment for the disease, but only alleviates the patient's serious condition.
Pain in a herniated disc can vary in intensity. Depending on this, the doctor prescribes a weakby efficiencypainkillers or strong drugs.
The simplest drugs are dispensed in pharmacies without a doctor's prescription, while strong painkillers - only on the recommendation of the attending doctor on the appropriate form.
Drugs prescribed for vertebral hernia can be divided into several main groups:
- non-steroidal anti-inflammatory drugs;
- muscle relaxants;
- narcotic analgesics;
- analgesics non-narcotic;
- sedatives;
- hormonal agents.
Treatment of vertebral hernia in practice is accompanied by complex therapy of the above groups of drugs with drugs that directly affect the cause of the disease, as well as drugs that affect symptoms of the disease, such as high body temperature, which is sometimes observed in postoperative period, swelling of painful places, high blood pressure, numbness.
Painkillers for spinal hernia are taken in a strictly recommended dose, determined by the attending physician. If the pain does not subside after taking the medicine, in no case should you increase the dose on your own, it is much safer to get a second consultation. Many drugs do not work together or can cancel each other out. When treating a spinal hernia, it is always important to consult a specialist.

Most medications that can be used to treat a hernia can cause side effects or addiction. Therefore, experts recommend using painkillers only when the discomfort cannot be tolerated.
Some drugs used for drug treatment vertebral hernia, not only anesthetize the painful areas of the spine, but also contribute to their recovery.
The use of non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs belong to the main group of drugs used in the treatment and elimination of pain in vertebral hernia. The list of drugs in this group includes:
- Ketorolac;
- Celebrex;
- Ketotifen;
- Diclofenac;
- Amidopyrine;
- ibuprofen;
- Movalis;
- fluibuprofen;
- Naproxen;
- Phenylbutazone;
- Surgama;
- Piroxicam;
- Aspirin.
If the treatment is agreed with a specialist, it makes no sense to be afraid, since contraindications are always taken into account, one of which is a problem with digestive system. Uncontrolled intake can provoke problems with the liver, the development of stomach ulcers, bleeding. In order to avoid possible discomfort or side effect, such drugs are prescribed simultaneously with drugs that can reduce Negative consequences their acceptance.
Most drugs on the list of non-steroidal anti-inflammatory drugs are not recommended for pregnant women, nursing mothers and patients. childhood. They are contraindicated in anemia, kidney disease, gastritis, ailments circulatory system, high pressure.
Side effects caused by non-steroidal anti-inflammatory drugs:
- nausea and vomiting;
- diarrhea;
- internal bleeding;
- dizziness;
- physical weakness;
- increased sweating.
What you need to pay attention to: after taking non-steroidal anti-inflammatory drugs, you will need to withstand a certain period, which is necessary to restore the body, in particular, the gastric mucosa. To minimize side effects drugs are often produced coated with a special protective shell.
In the pharmacy network, you can find drugs in this group in the form of capsules, tablets, ointments and gels. Intervertebral pain syndrome is quickly relieved by non-steroidal anti-inflammatory drugs: Voltaren emulgel, Fastum gel. However, they may cause allergic reactions, urticaria on the skin, especially in people who are allergic to the drug or its component.
The positive effect of hernia treatment with this group of drugs is observed when combined with rational nutrition, in a healthy way life.
Non-narcotic analgesics

If anon-steroidal anti-inflammatory drugsunsuitabledue to the patient's contraindications, then pain relievers from the group of analgesics help to relieve the pain syndrome, which gives with a vertebral hernia to the chest, lower back, and shoulders. Tilenol, Paracetamol, Acetaminophen tablets are presented on the pharmaceutical market. Their action may not be enough, so the doctor prescribes them in combination with other medicines. It is not recommended to increase the dose, as there is a risk of overdose or poisoning.
The analgesic effect lasts for several hours (from five to eight).
Relaxants in the treatment of vertebral hernia
What else can relieve the pain of a hernia of the spine? It is possible to do this with the help of muscle relaxants such as Sibazon, Valium, Sirdalud, Mydocalm, Balclofen. Their action is to remove muscle spasm in the lower back, due to this, blood circulation improves.
Antidepressants and corticosteroids
Pain can also be relieved with antidepressants.especially when the pain is psychogenic in nature. Prolonged pain syndrome leads to the fact that a person becomes irritable. Means affect the central nervous system, mental condition the patient, depressing the pain, enable the patient to fully relax due to the fact that after taking it you want to sleep. It is optimal to prescribe drugs to this group along with the rest.
With exacerbations of a vertebral hernia and a deterioration in a person's condition, doctors prescribe drugs - corticosteroids. Since the funds are hormonal, they are used in the most extreme cases and with a pronounced pain syndrome caused by inflammation. A separate indication for use is the ineffectiveness of non-steroidal anti-inflammatory drugs. Hormonal include: Decadron and Methylprednisolone, Dexamethasone. When prescribing, a number of contraindications are taken into account, the main of which are hormonal disorders, problems with the digestive system, pregnancy, lactation.
Blockade with hormonal drugs
In the absence of the effect of the applied general treatment the doctor may recommend a blockade with a hormonal drug. It acts on a specific area, reducing the intensity of the pain syndrome by reducing the inflammatory process. Before the procedure, the injection site is anesthetized with novocaine, and the procedure itself can also be performed. After that, the doctor may introduce such means as: Kenologist, Diprospan, Flosteron. The procedure can be repeated several times depending on the effect obtained.
It is impossible to get carried away with such blockades, they lead to the development of degenerative processes at the injection site. Over time, the duration of the therapeutic effect is reduced, which requires a second procedure. In the worst case, there is a high risk of infection.
Synthetic drugs
 In situations where the pain cannot be physically endured, patients are prescribed narcotic drugs of synthetic origin. AT medical practice such means are used: Fentatin, Codeine, Tramadol, Morphine. They are addictive, so they are taken under the strict supervision of the attending physician and only if no other treatment, including surgery, is possible. You won’t be able to buy them freely at the pharmacy either, for this there must be a special prescription, since the funds belong to a group of special strict accounting.
In situations where the pain cannot be physically endured, patients are prescribed narcotic drugs of synthetic origin. AT medical practice such means are used: Fentatin, Codeine, Tramadol, Morphine. They are addictive, so they are taken under the strict supervision of the attending physician and only if no other treatment, including surgery, is possible. You won’t be able to buy them freely at the pharmacy either, for this there must be a special prescription, since the funds belong to a group of special strict accounting.
Conclusion
Stopping pain in vertebral hernia begins with slow-acting drugs with minimal side effects. If they do not give the desired result, doctors prescribe stronger pain medications.
In many cases, vertebral hernia requires operable intervention, andlongtaking painkillers can only make it worsesituation, bringing the patient to the operating table. For this reason, the treatment of spinal hernia is performed in a medical facility by competent specialists.not only with the use of analgesics.
All pain medications applicable for vertebral hernias are not safe drugs, to independently prescribe them to yourself is categorically contraindicated. You should not experiment on personal bitter experience, listen to the advice of neighbors or friends. Only a doctor knows which remedy and in what dosage can help with a serious health condition.
Self-activity in the choice of painkillers can lead to dependence on antidepressants, narcotic substances, which is highly undesirable. Improper use of drugs may not relieve pain, but provoke the progression of the disease, resulting in paralysis of the limbs. Therefore, it is so important to take medicines as prescribed and only on the recommendation of the attending doctor.
