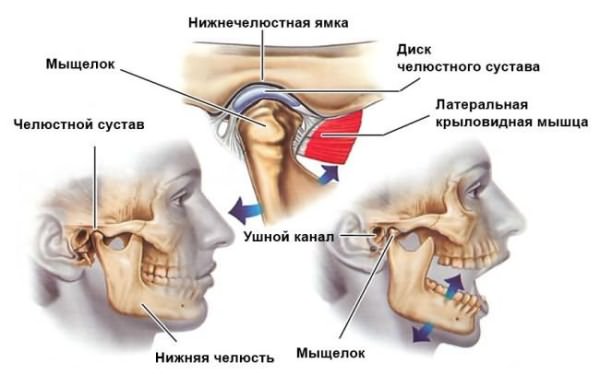
Temporal mandibular joint(TMJ) is a paired formation located behind the earlobe. It connects temporal bone skulls with lower jaw and ensures its movement in three directions. Any abnormalities in its functioning or neighboring structures cause pain, discomfort and impaired articulation.
The jaw joint belongs to the combined type: movements from the left and right side are carried out synchronously. It consists of:
Malfunction in the temporomandibular joint or temporomandibular joint dysfunction is a set of symptoms that can occur in very different ways, combining one or more of the following. Painful manifestations. - joint manifestations: joint sounds, painful restriction or no opening of the mouth, discomfort in chewing and eating, joint instability sensation, blocking the mouth closed or otherwise blocking the open mouth. - other manifestations such as ringing in the ears or neck.
The various mechanisms that cause temporomandibular joint malfunction are complex, but various risk factors are known and are often confused, leading to malfunction. They are often associated with the stress of daily life and deviations from dental articulation. 5 - hyperlaxity is due to the presence of ligaments, too loose, too stretched. This is typical for young women.
Joints move in three planes:
- frontal - up and down;
- sagittal - forward and backward;
- vertical - in the lateral direction.
Blood is supplied by branches of the external carotid artery, and its outflow is provided by the venous network of the jaw. Lymph drainage occurs in cervical lymph nodes. Because of this, their increase is one of the symptoms of TMJ inflammation.
This leads to the fact that maximum mouth opening is too important. This contributes to clogging of the open mouth. 6 - Rheumatic disease can occur in jaw joint. The jaw joint is a joint located in the front of the ear that connects top part jaws to skull.
This articulation has the peculiarity of representing the meniscus. When someone opens their mouth, the condyle rotates and moves forward. The meniscus follows the movement, moving forward. What are various stages diseases? The first stage of the disease corresponds to the pure muscular stages. Abnormalities in muscle function responsible for pain are caused by muscular compensations for positional disorders of the mandible. These positional abnormalities in the mandible are associated with articular joint problems and parafunctions.
Important! The innervation of the TMJ is provided by the ternary nerve. Therefore, the reason why the jaw hurts may be hidden in pathologies of other parts of the face.
Causes of pain
Pain in the jaw joint may occur due to:
- Mechanical injuries: bruises, fractures, dislocations. They are accompanied by hemorrhage into the joint cavity, rupture of the capsule, ligaments, and cracks of the superficial bones.
- Infection. Occurs due to the penetration of pathogenic microorganisms into the cavity. Infection is possible when:
3. Systemic inflammatory diseases:
These muscle symptoms, these pains are aggravated by stress and anxiety. At this stage, treatment is never surgical; occlusion devices usually eliminate pain. The disc ends up bulging forward. For example, ear pain is often associated with spasm of the lateral pterygoid muscle. This muscle is distinguished by the fact that it is inserted into the anterior part of the articular disc. Its spasm, in addition to causing pain, draws the meniscus forward and thus can cause or aggravate disc displacement.
Stretching of the disco-ligamentous structure results in the appearance of dislocations and mandibular subluxations and joint instability. Articular symptoms associated with disc displacement appear. Clicks translate the disk offset being reduced. Over time, the disc moves more and more forward until it eventually prevents the mouth from opening. The clicks disappear, and pain associated with opening the mouth appears. This is the stage of irreducible movement of the disk.
- arthritis – inflammatory pathology caused by viruses and infections, it can affect any joint: jaw, knee, elbows, shoulder, ankle;
- arthrosis – the jaw joint is subject to destructive damage;
- systemic lupus erythematosus - antibodies begin to attack the intracellular structures of the body, but no structural deformation occurs;
- gout - accompanied by impaired excretion or increased formation of uric acid, which accumulates in the tissues.
4. Neoplasms:
Lack of interposition of the articular disc ultimately leads to transformation of the ligament and disc structure, and parallel wear phenomena occur. articular surfaces. This is temporomandibular osteoarthritis. This typical evolution is not always followed. Some patients with reduced disc slippage will never experience disc slippage. Some patients with irreversible disc slippage will never progress to osteoarthritis, while others develop directly into osteoarthritis.
- benign: adamantinoma, osteoma, osteoblastoclastoma;
- malignant: sarcoma, cancer.
Important! The TMJ can also hurt due to bite defects, advanced carious lesions, neuralgia trigeminal nerve, arteritis of the facial artery, incorrectly installed orthodontic (braces) and orthopedic structures (bridges, dentures).
What is the origin of pain and its treatment?
The evolution of temporomandibular dysfunction is unstable, more or less long-term in accordance with mechanical, functional, constitutional and psychological factors. There are two types of pain: - they are of muscular origin most often and initial stages diseases. They are associated with muscle spasms and contractures. - They become articular with the development of the disease and the appearance of joint lesions. In fact, this is the stage where they most often become confused.
It is the difference between these two types of pain that determines success and treatment. Initially, your practitioner most often cannot tell whether the pain is due primarily to muscle spasms or joint disorders unless you have a completely normal joint examination or if, on the contrary, the joint problem is egregious such as severe osteoarthritis.
Symptoms
Pain in the temporomandibular joint is local or radiating. Local signs of dysfunction include:

TMJ dysfunction is also accompanied by radiating pain in the head, facial muscles, ears, neck and upper back. Often, diseases of the jaw structures lead to impaired auditory and visual functions, dizziness, and disorientation in space.
Your oral surgeon will usually begin treatment with occlusion devices. This treatment is capable of eliminating pain of muscular origin and regulating minor and still reversible joint disorders, but is not effective in eliminating pain associated only with a joint disorder that has already developed.
This treatment, which should last 2 to 3 months, can make the difference between the two causes of pain. Nine times out of ten, this occlusion device treatment is effective and solves your problem because pain is most often associated with muscle spasms and minor joint disorders after a muscle spasm. Even if it persists after treatment and after the pain has gone, the helmet, reflecting a minor joint disorder, is tolerated because it is clearly not the cause of your pain.
Important! Due to radiating pain, disturbances in the functioning of the TMJ are often confused with pathologies of other organs: migraine, periodontal diseases, dental diseases, disruption of the mechanism for equalizing intra-ear pressure.
How to relieve pain?
Cure diseases yourself temporomandibular joint impossible. Correct therapy requires careful diagnosis and identification of the exact cause of inflammation. However, a number of measures will help reduce pain syndrome before visiting the doctor:
The resulting result can then be stabilized by treating the articulated tooth anomalies to position the joint and mandible in the most stable position with the least amount of traumatic impact possible. Less commonly, treatment of the occlusal apparatus remains ineffective. Then we know that pain is mainly due to the general disorder that you are present with. Treatment of pain then requires treatment of the syndrome. An indication for surgical treatment is provided.
Why is my jaw popping into my mouth?
Nerve complications: - Nerve contusions passing close to teeth depend on specific anatomical situations. The presence of a latch when opening the mouth reflects the presence of displacement in front of the joint disc. In a closed mouth, the meniscus, advanced forward, is not inserted between the jaw and the skull.
- Applying cold. Ice wrapped in a towel or a handkerchief moistened with cold water is applied to the affected area. The procedure time should not exceed 15 minutes, the subsequent session is carried out at least an hour later.
- Warm compresses. The jaw joint is warmed with a bag of salt, paraffin, and a damp heated towel.
- Taking analgesics. They will help you temporarily remove sharp pain. “Ketanov”, “Nurofen”, “Nise” are recommended.
- Reduce the load when chewing. It is necessary to eat non-solid foods: cereals, soups, grated fruits, vegetables, fermented milk products. It is also better to sleep on your side or back to avoid squeezing your jaw while resting.

On the other hand, in open mouth the anatomy becomes normal again. The meniscus is reinserted between the condyle and the skull. Schlamming reflects the passage of the condyle under the meniscus. The presence of painless and uncomfortable isolated temporomandibular joint tethering does not require treatment.
Mouth locks are more or less repeated episodes of painful restrictions on opening the mouth. They must be: - either moving in front of the meniscus. When opening the mouth, the condyle cannot stroke under the meniscus, displaced and adjacent to its posterior part. Opening restrictions are painful, but generally moderate. In this case, there is often a breakdown in which more or less repeated episodes of closed mouth locking occur. 2 - or into the meniscus, literally “glued” to the skull, which does not move at all when the mouth is opened.
A warm compress relieves pain.
Important! If not known the real reason, because of which the jaw joint hurts, warm compresses are excluded from the list of what can be done - they accelerate the spread of infection.
Diagnostics
The initial diagnosis of TMJ dysfunction is carried out by a general dentist. Depending on the cause of the lesion, he may refer you to a specialist in another direction:
This is the phenomenon of a fixed disk. The restriction is very painful and usually severe. The patient usually enters this stage of the disease without prior joint slap. There is actually inflammation of the joints that has altered the normal lubricating fluid of the joint. The friction between the disc and the articular surfaces increases until they become too important. The disc is then fixed and recorded on tape.
What is jaw dislocation?
In this case, it is interesting to practice arthroscopy-washing the joint when the blockage is not quickly removed. This allows the meniscus to “release”, restoring normal joint pressure and normal lubrication to the joint. Sometimes the jaw moves too much when opening the mouth and is a luxury. The pastry chef protrudes forward from its normal joint cavity.
- surgeon;
- traumatologist;
- neurologist;
- orthopedist;
- gnathologist;
- rheumatologist;
- otolaryngologist.
During the examination, the patient is initially interviewed, visually examined and palpated. To clarify the cause of dysfunction, you need to do:
Treatment
Treatment for TMJ dysfunction depends on the type of pathology and the cause of its occurrence. There are several methods of therapy:
There are two possibilities: 1 - either the dislocation spontaneously decreases. This is then a subluxation, which often manifests itself as a feeling of joint instability. This is facilitated by joint hyperlaxity. 2 - or the dislocation remains. That's when it's real dislocation, requiring a reduction in urgency. It is very different from a meniscus dislocation or meniscus slip.
What is temporomandibular osteoarthritis?
Just like the hip or knee, it reflects the wear and tear of all joint structures. This is manifested by joint pain, aggravated by chewing, squealing noises, which are associated with the friction of two worn surfaces of the joint against each other. When this is important, it causes a painful restriction in mouth opening.
- Immobilization. It is used for traumatic lesions after appropriate measures: reduction of dislocation, comparison of bone fragments. Immobilization of the jaw is also necessary if there is a possibility that the jaw joint may become dislodged or if a fracture is suspected.
- Drug therapy. Aimed at eliminating pain and suppressing the growth of pathogenic microorganisms. Appointed:
- analgesics: paracetamol, Nurofen;
- non-steroidal and steroidal anti-inflammatory drugs: Diclofenac, Nimesil, Affida Fort, Prednisolone;
- antibiotics: Amoxicillin, Tetracycline;
- antifungal agents: Nystatin, Fluconazole;
- cytostatics: Methotrexate, Sulfasalazine.
3. Physiotherapy. Apply after removal acute symptoms. Most often prescribed:
Temporomandibular osteoarthritis sometimes occurs spontaneously, sometimes it may be an evolutionary result of old temporomandibular dysfunction or true rheumatic disease. Conventional occlusion device treatment is much less effective than the general case. Surgery is often necessary, but prosthetic rehabilitation of posterior asthenia, often associated with temporomandibular osteoarthritis, remains essential.
What are occlusal devices?
Occlusal dipositives can be presented in different ways. There are two types of occlusion devices most widely used. Occlusal groove. This is a kind of "tooth guard" which is wedged into one of the two dental arches by one of these faces and whose other face is smooth. - retro cutting bite plan. This is a device that wedges into the palate and prevents the teeth from snagging because it has extra thickness behind the incisors. These occlusal devices interfere with the dental joint. When anomalies of the articulated teeth occur at the onset of symptoms, these occlusal devices allow their temporary elimination and therefore the disappearance or improvement of pain.

4. Surgical intervention. Used when other treatments fail positive result or with extensive damage (displaced fractures and multiple fragments). Infectious processes, for example, purulent arthritis, are also indications for surgery. The technique consists of opening the cavity, cleansing it of pus and areas of necrosis.
They also have a muscle relaxing effect. In fact, it becomes impossible to clench the teeth, this prevents the jaw muscles from pushing out and gives way, over time, to vicious circles that maintain muscle spasm. Disappearance muscle spasms causes pain to disappear.
Moreover, by inhibiting dental articulation, they do not allow the parafunds to express themselves. With the help of these devices, the temporomandibular joint and the lower jaw are rebuilt into an ideal position, without being limited by the traumatic position associated with dental malocclusions.
Important! As complementary therapy appoint therapeutic exercises, increasing jaw mobility.
Possible complications
The lack of correct treatment for TMJ diseases can lead to structural changes in the joint itself, adjacent tissues and further spread of infection. Possible complications include:
- Loss of mobility – ankylosis. Occurs due to fusion of articular surfaces. The causes are tissue proliferation during infectious processes and after fractures.
- Destruction of structural parts. Occurs against the background of damage by staphylococci and streptococci. Leads to complete or partial limitation of mobility.
- Meningitis. The membranes of the brain become inflamed if the infection begins to spread along the ascending path.
- Phlegmon. The purulent process in fatty tissue develops against the background of inflammation with a decrease in the body’s immune forces.
- Sepsis. Penetration of infection into the bloodstream and its further spread.
The jaw joint is affected as a result of trauma, infection and the development of systemic diseases. Due to the features immune system and natural wear and tear, this pathology is often observed in older people. Its treatment is carried out only by a specialist after a thorough examination and determination of the cause of the inflammation.
Diagnosis of TMJ lesions is complicated by the fact that this pathology has a lot of symptoms. But some of them can be called classic - those that affect the TMJ joints themselves, ears, head, face and teeth. Since there are no nerve endings in the joints, when their function in this area is impaired, a person does not experience pain. It occurs in the ears, in the neck, head, or in trigger points, which are compactions in the muscles (masticatory, temporal, sublingual, temporal, cervical) - pain is felt when pressing on them. At the same time, there is a noise in the ears, a crunch in the joints when opening the mouth.
The most common symptom is clicking in the lower jaw joint, which is not always accompanied by painful sensations. The sound made by the jaw can be heard by others. If the jaw clicks, it means that the disc is displaced and the muscles that support the lower jaw while chewing food are unnaturally tense. The consequence of this tension is pain in the muscles, face, head and neck.
Blocking or locking of the TMJ is a condition in which the joint moves unevenly due to disorders that have occurred in it. The person notices that the lower jaw opens unevenly, as if it is catching something. And in order to open your mouth wide, you first need to move your lower jaw in one direction or the other, sometimes you have to do this until a click is heard at the point of its “unlocking”.
Due to the proximity of the TMJ to ears, its defeat often causes ear pain, congestion, and even hearing loss. Ringing in the ears can be caused by both joint disorders and pain management with medications (aspirin, ibuprofen).
Prevention
Prevention is timely and high-quality treatment and dental prosthetics, bite correction, timely seeking help from a doctor after an injury.
