The knee joint is formed by two long tubular bones: the femur (top) and the tibia (bottom). In addition, in front knee joint there is a small rounded bone called the patella or patella.
Two spherical elevations are located at the bottom of the femur and are called the femoral condyles. They are covered with articular cartilage and form the articular surface of the femur. The femoral condyles are in contact with the flat surface of the tibia. This surface is called the tibial plateau.
Therefore, the injury that is valued in radiographs is serious, deep. This improves its performance by injecting a contrast fluid into the joint. It is also very effective in detecting other related knee injuries. However, there is a percentage of cases that avoid diagnosis.
If loose bodies are suspected, they should be removed by arthroscopy. The remaining cartilage injuries should be treated initially with a specific physical therapy program. In some cases, the doctor prescribes templates that adjust the support of the affected limb, freeing the knee from effort.
The structure of the knee joint: 1 - femur; 2 - patella; 3 - articular cartilage; 4 - tibia.
The tibial plateau consists of two halves: the medial tibial plateau is located closer to the midline of the body, and the lateral plateau is outward from it.
The patella slides along a special groove formed by the femoral condyles called the patellofemoral groove. The fibula is not involved in the formation of the knee joint. It is located on the lower leg lateral to the tibia. These bones are connected to each other through a small, inactive joint.
When these methods fail, arthroscopy, the simplest method, should be considered. surgical treatment with fewer complications. Perforate with a small drill at the bottom of deep ulcers to allow the bone to bleed and allow better healing. If the cartilage fragment is recently detached and large enough, it can be tied to the crater with a special screw.
- Remove loose bodies.
- Clean the edges of the sores.
- Flush the joint with sterile saline to improve cartilage turnover.
Articular cartilage covers the articular ends of bones at any joint. The thickness of the articular cartilage in the knee joint is about 5-6 mm. This fabric white color with a shiny, very smooth surface, has a dense elastic consistency. The function of articular cartilage is to reduce friction forces during movement in the joint, as well as to absorb shock loads. Thus, articular cartilage is needed where there is movement of two bony surfaces relative to each other. At the knee joint, articular cartilage covers the articular ends of the femur and tibia, as well as the posterior surface of the patella.
In the cartilage of the thigh or lower leg, you can try to transplant fragments of healthy cartilage from the periphery of the knee, forming a mosaic; or grow cells of this cartilage and then layer on the ulcers. Change position patella in cases of cartilage damage. . The results are often disappointing.
How to live with a cartilage injury?
The patient should limit their work and sports activities depending on the evolution of symptoms and their doctor's examinations. It is wise to monitor periodically once symptoms have resolved to prevent the onset or development of osteoarthritis. Roberto Palacio Gonzalez, specialist in orthopedic and trauma surgery, Dr. Salvador Pertusa Martinez, family doctor.
The ligamentous apparatus also includes the lateral and cruciate ligaments.
cruciate ligaments located in the cavity of the knee joint. Their ruptures are caused by transcendental movements in the knee joint. Anterior cruciate ligament (lat. lig. cruciatum anterius) starts from the posterior part of the inner surface of the external condyle (bone protrusion) of the femur, crosses the cavity of the knee joint and is attached to the anterior part of the anterior intercondylar fossa of the tibia also in the joint cavity.
The knee is the most complex articulation of the human skeleton. On the one hand, judging by the surface of the joint, this may seem like a very mobile articulation; on the contrary, the rich ligamentous apparatus from which it is supplied reduces its movements only to the point of flexion. The classification of this articulation is also difficult.
The thighs, with their condyles and the surface of the patella, the knee and lower legs, with their consile surface, are part of the knee joint. Plywood, on the other hand, does not enter into it, only articulating from the lower leg. The knee is an angular ginglimo, with two degrees of freedom in flexion and one in extension.
This ligament stabilizes the knee joint and prevents the lower leg from moving excessively forward, and also holds the lateral condyle of the tibia. Posterior cruciate ligament of the knee (lat. lig. cruciatum posterius) starts from the anteroposterior part of the lateral surface of the internal condyle of the thigh, crosses the knee joint and attaches to the posterior intercondylar fossa of the tibia. It stabilizes the knee joint and keeps the lower leg from moving backward.
it flat bone with two surfaces, one front and one back, three sides and a bottom; its form, however, is highly variable. The anterior surface is very rich in food openings; It is also very curved, with longitudinal reliefs more or less pronounced depending on individual individuals, and which are areas of insertion of the tendinous muscle of the quadriceps femoris. In the proximal region, the surface is smoother, where the middle and right thigh muscles fit.
The upper part is divided longitudinally by a relief into two articular surfaces through which the patella is pivotally connected to the patella of the femur. The articulation of the femur of the femur is formed by an expanded distal epithelium, consisting of two warts, medial and lateral, fused in the diaphysis and diverging from the side in the lateral direction: an intercondidal fossa was obtained. Above and laterally, each condyle has an epicondyle, the upper medial part of which forms a projection: a tubercle that inserts part of the large muscular muscle.
Ticket 38
Ankle joint: shape articular surfaces, movement.
Ankle joint(lat. articulation talocruralis) - the articulation of the bones of the lower leg with the foot - the movable connection of the tibia, fibula and talus bones of a person. Complicated in structure, block-shaped in shape, formed by the articular surfaces of the distal (located further from the body) epiphyses of both tibia, covering the talus block with a “fork”. The tibia is adjacent to the upper articular surface of the talus, and on the sides are the articular surfaces of the outer and inner anklebones.
Before the distal epidemic, there is a smooth triangular area, the surface of the patella, which is articulated with the patella. The articular surface of the femur, consisting of the lower surface of two muscle tissues, is smooth and articulated with the tibial plate, that is, with the upper surface of the proximal epithelium of the leg, while it does not have contact with the pelvis.
The proximal epithelium of the tibia consists of two condylomas, intercondylomas, tibial tubercle, and two intercondylomas. The lateral condyle has a wide surface, convex and irregularly rounded, almost flat surface. Directly to the lateral condyle there are two pyramidal projections, the lateral and medial intercondyle tubercles, which protrude above the two condyles and where their anterior and posterior margins converge. The base of the two tubercles occupies about half the thickness of the tibia, and together they form the height of the intercondidium, and the remaining notches make up the anterior and posterior intercondylloid regions, from which two crossed ligaments arise.
The following movements are possible in the joint:
frontal axis - flexion and extension of the foot;
sagittal axis - slight abduction and adduction.
The tibia and fibula enclose the talus block like a fork. The articular capsule behind and on the sides is attached to the edges of the articulating surfaces, and in front it retreats from them by half a centimeter. Ligaments are located on the lateral surfaces of the joint:
Usually, the lateral field is said to be inserted, since the inserted membrane is inserted, which occupies the space between the tibia and the featherbed. There is a slight curvature behind the medial condyle that can be inserted into the tendon of the semimembranous muscle.
Their functions are diverse: they protect the articular cartilage of the bony heads by reducing stress, stabilizing the joint, and expanding the articular surface of the tibial plates. Both menus fit into the intercontact emphysema of the leg. A fibrous cap is inserted on the posterior face of the femur 1 cm above the limit of the articular cartilage; it adheres to the contour of the patella and is attached below to the plates of the tibia, a few millimeters below their cartilaginous covering.
tibial-navicular part (lat. pars tibionaviculare) is attached to the navicular bone of the foot,
tibiocalcaneal (lat. pars tibiocalcanea) is attached to calcaneus and
The knee flexors are instead contained at the back of the thigh and are nearly all biorbital. These include: femoral biceps, semitendinoids, semimembranes, internal straight line, sartorius. The rotating muscles of the knee are external rotators and internal rotators.
Reasons why the knee is the most treated articulation with infiltration therapy
The knee joint is undoubtedly the most frequently used anatomical area for infiltration therapy. This is explained various reasons: the knee is the most common location degenerative changes and regardless of the course, patients who suffer tend to approach the therapist very soon because of the pain; line and articular spaces are easily accessible and perceived through the skin; In the case of intra-articular injections, the drug quickly diffuses and integrates the entire synovial surface, since the articular surfaces are predominantly flat.
anterior and posterior tibial-talar parts (lat. pártes tibiotaláres anterior et posérior) attached to the talus.
on the outside of the joint are the anterior and posterior talofibular and calcaneofibular ligaments - they all diverge in a fan-like manner, starting at the lateral ankle: the anterior talofibular ligament (lat. ligamentum talofibulare anterius) is attached to the neck of the talus, the posterior talofibular ligament (lat. ligamentum talofibulare posterius) - to the posterior process of the talus, and the calcaneal-fibular ligament (lat. ligamentum calcaneofibulare) goes down, ending on the outer surface of the calcaneus;
Stability of the knee is provided by powerful ligaments: oval ligaments and crusaders, as well as the same muscle. The cruciate ligament, collateral ligaments originate from the epicondyle of the femur and fit on the tibia and the head of the fibula, the patellar ligament that connects the patella to the tibial tuberosity.
The knee extensor muscle is formed by the femoral quadriceps muscles located in front of the thigh. It consists of four muscular ventricles that connect through a common terminal tendon at the anterior tubercle of the leg. The large middle, large exterior and extensive interior are monoarticular, the anterior right is biarticular.
on the inside of the ankle joint is the deltoid (medial) ligament (lat. ligamentum deltoideum seu mediale), which begins at the inner (medial) ankle and is divided into four parts:
Movements in ankle joint - flexion and extension, pronation and supination, rotational movements.
Lifting force of the muscles. Factors affecting the magnitude of the lifting force.
muscle strength determined by the magnitude of the load that the muscle, with its maximum contraction, can lift to a certain height. This force is called lifting force muscles. The strength of different muscles is not the same. It depends on the number of muscle fibers on the cross-sectional area of these fibers. Comparing the equal size fusiform muscle with a longitudinal direction of long muscle fibers and the pennate muscle with an oblique direction of a larger number of short muscle fibers, we will find that the pennate muscle is stronger. An indicator of muscle strength is its physiological cross-section the cross-sectional area of all its muscle fibers (Fig. 32). The size (size) of a muscle is characterized by its anatomical cross-section cross section of the muscle of its widest part.
Classification of injection modes
The latter, however, unless strictly necessary for specific cases, is generally not used as it is technically more complex with no specific therapeutic benefits. Depending on the indication, there are many points on the knee that can be effective for injections, which can belong to two main categories: internal or peri-surgical; in the latter case, the drug can be administered at the level of muscle structures, tendons, ligaments, nerves or subcutaneous.
This access route is used in case of pain, spillage or limited mobility. The patient is stretched supine with the knee extended, and the superior pole of the patella is sought, and the lateral edge of the femoral condyle. The point of less force between the latter and the top of the crown - about 1 cm below the super-outer edge of the roll - represents the injection site. The needle is inserted perpendicular to the skin surface, about 1-2 cm below the top edge of the sheet. It may be helpful to perform a subluxation of the roll so that the needle fully penetrates the skin if the patient does not feel painful.
Rotational force of the muscle depends not only on its physiological diameter and lifting force, but also on the angle of attachment of the muscle to the bones. The greater the angle at which a muscle attaches to a bone, the greater the effect it can have on that bone. Blocks are used to increase the angle of attachment of muscles to bones.
Ticket 40
Types of muscle work (static, dynamic, yielding, overcoming, holding)
Frontal access is indicated in patients with gonadal anomalies, arthritis, and after traumatic internal injuries of the knee. The patient can stand on their back with the knee bent at 90°, or sit on the edge of the bed. The injection site is represented by a point of less resistance at the superior point, consisting of the ligature ligament, the lower edge of the femoral lateral condyle, and the upper edge of the tibial plate. The needle is inserted slightly higher and parallel to the tibial plate, slightly inclined in the medica, to the intercontinuous throat.
Care must be taken not to strike the femoral cartilage as this may cause pain in the patient, persistent for several days and sometimes accompanied by swelling. Another way to identify the injection site is as follows: the patient is palpated and marked with medial and lateral articular lines, which are combined with the "first auxiliary line". Never force a drug. It is easily identified as it is located superficially above the crown. This is at the same time the repair point and injection site indicated for the treatment of pre-taternal borsitis.
Static muscle work- the process of muscle contraction necessary to maintain the body or its parts in space. It is characterized by the fact that muscle tension develops without changing the length of the latter and without active movement of the moving links (limbs) and the whole body. In the process of labor, static work is associated with fixing tools and objects of labor in a stationary state, as well as giving a person a working posture. Static muscle work is a process in which muscle cells are excited, all muscle fibers are tensed, but at the same time there is no contraction them, which means that the muscle remains in a tense elastic state for a certain period of time. Such static muscle work ensures the preservation of the desired position of the human body or its individual parts for a certain time.
The patient should be in the supine position, with the joint extended. The needle is inserted perpendicular to the skin surface. In the case of suprapubic bursitis, the top point above the patella consists of a notched pouch. Injection with the patient in the same position as described above, and which requires relaxation of the quadriceps muscle, should be performed in this bag, keeping in mind the superolateral and superomedial margins of the crown. In this case, the needle is inserted parallel to the plane of the skin, just above the top edge of the patella.
In the presence of exudates, it is necessary to aspirate them before taking the drug, which should not be performed if the aspirate appears to be infected. In patients with tendonitis and paw tendon bursitis, for tendon injection, the medial line of the knee joint, in which the so-called goose foot insertion of the sartorial muscles, is graceful and semi-rigid. The drug should be injected close to the tendon insertion of the sartorial muscles, graceful and semi-rigid and deeply close to the semimembranous muscle.
During static work, metabolism increases, energy consumption increases, although to a lesser extent than during dynamic work. Static work is more tiring than dynamic work, since muscle tension lasts continuously without pauses, not allowing them to rest. In addition, during static work, blood circulation in working muscles is difficult, there is a decrease in volumetric blood flow in them, a decrease in oxygen supply and a transition to anaerobic energy supply with the accumulation of a large amount of lactic acid, in proportion to the magnitude of the static voltage.
Static work, depending on the nature of the activity of the muscles, can be divided into two types:
Static work to hold tools and objects of labor in the process of performing a production operation by a person. This is achieved by tetanic muscle contraction, which occurs under the influence of powerful nerve impulses.
Static work aimed at maintaining the posture. This work is provided by tonic contractions, it is characterized by low energy costs and can last for a longer time. Nothing tires us more than static muscle work.
Dynamic muscle work, as the name itself indicates, is the work of movement. The most characteristic examples of such work are running, sawing firewood, hand mowing, playing lawn tennis. During dynamic work, the muscles contract rhythmically, alternately flexors and extensors. For example, when sawing wood, the arm flexes due to the contraction of the biceps, while actively spending some energy, but then it passively extends due to the active contraction of the extensor. Thus, the muscles either work or rest. If this shift will be more and more accelerated, then the active contraction of each will also become more frequent. According to the frequency and strength of the contraction, the expenditure of energy will increase, and, consequently, the degree of muscle fatigue.
Retention work performed due to muscle tension without changing their length (isometric mode tension). It is typical for maintaining a static posture of the body, holding an object (eg, barbells, dumbbells), etc.
Overcoming work performed due to a decrease in the length of the muscles during their tension (myometric mode tension). The overcoming work of muscles during the performance of motor actions occurs most often. It makes it possible to move one's own body or any load in the appropriate movements, as well as to overcome the forces of friction or elastic resistance (for example, flexion-extension of the arms in emphasis on the uneven bars).
Yielding work performed due to an increase in the length of a tense muscle (plyometric mode tension). Due to the inferior work of the muscles, depreciation occurs at the moment of landing in jumps, running, etc. Often, in the inferior phases of the movement, the maximum magnitudes of the force are manifested. In particular, it was found that in the yielding mode, the muscles can show strength by 50-100% more than in the holding and overcoming modes.
Ticket 41
One-, two- and multi-joint muscles. features of their work.
A monoarticular muscle attaches to adjacent bones and acts on one joint. Two- and multi-joint muscles are most often located more superficially, have longer tendons that are thrown over two or more joints. Some muscles do not move over the joints and do not act on them. They are only one end attached to the bones (facial, muscles of the tongue, perineum), the other is woven into the skin or other tissues.
Ticket 42
Muscle tone and condition.
Tone (from Latin tonus - tension) is a reflex muscle tension, which depends on the nature of the nerve impulses reaching them (neuromuscular tone) and on the metabolic processes occurring in them (own muscle tone). Normally, the muscle is not completely relaxed. This is due to the fact that in response to the efferent impulse coming from the brain, and to the afferent one, due to irritation of the proprioreceptors, the striated muscles are in constant tension (tonus), which is commonly called contractile or phasic muscle tone. From contractile muscle tone and arising from its increase in spasticity should be distinguished by plastic muscle tone, characterized by muscle rigidity. With an increase in muscle tone according to the plastic type, muscle resistance, detected during passive movements, is uniform, as in the flexion-extension of a lead tube (a symptom of a lead tube). Plastic muscle tone is determined by the state of extrapyramidal subcortical structures (see Chapter 5). Muscle tone provides preparation for movement, balance and posture. When maintaining a fixed posture and during movements, there is a contraction of some muscles and relaxation of others. The ratio of muscle tone, agonists and antagonists (their reciprocity) was studied by the English physiologist C. Sherrington (Sherrington Ch., 1857-1952). If the innervation of the muscle is disturbed, its tone decreases. If the peripheral motor neurons and the spinal reflex arcs associated with them are preserved, and the control over the state of peripheral motor neurons from the cerebral structures is impaired, muscle tone usually increases. The state of muscle tone is assessed in the process of observing the active movements of the patient, when examining and feeling his muscles , with passive changes in the position in space of parts of the patient's body. Decreased or absent muscle tone is called hypotension or muscle atony; high muscle tone - muscle hypertension. With paralysis and paresis, contractile muscle tone changes. In the case of hypotension (and even more so atony), the muscles are sluggish, flabby, their relief is not contoured, with passive movements there is no muscle resistance, while the range of motion can be excessive (Olshansky's symptom), the joints are loose. Over time, in such cases, muscle hypotrophy develops.
Ticket 43
Trunk extension (back muscles).
Full text search:
Home > Abstract >Medicine, health
Kneejoint(articulatio genus)
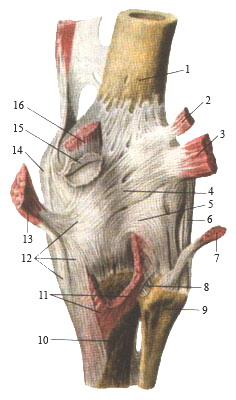
Knee joint, right. Front view.
The joint capsule has been removed. The tendon of the quadriceps femoris and the patella are lowered down.
1-patellar surface of the femur; 2-posterior cruciate ligament; 3-anterior cruciate ligament; 4-medial condyle of the femur; 5-tibial collateral ligament; 6-transverse ligament of the knee; 7-medial meniscus; 8-ligament of the patella; 9-patella; 10-tendon of the quadriceps femoris (cut off and lowered down); 11-interosseous membrane of the leg; 12-head of the fibula; 13-anterior ligament of the head of the fibula; 14-tendon of the biceps femoris; 15-lateral meniscus; 16-fibular collateral ligament; 17-lateral tibial condyle
The structure of the knee joint
The knee joint, articulatio genus, is the largest joint of the human body, complex in structure. Three bones are involved in the formation of the knee joint: the femur, tibia and patella.
Articular surfaces:
Articular surface of the femur formed by the medial and lateral condyles, which have an ellipsoid outline, and the patella surface on the anterior surface of the distal femoral epiphysis.
Superior articular surface of the tibia represented by two oval depressions that articulate with the condyles of the femur.
Articular surface of the patella, which is involved in the formation of the knee joint, is located on its posterior surface and articulates only with the patella surface of the femur.
The articular surfaces of the tibia and femur are supplemented with intra-articular cartilage: medial and lateral menisci. They increase the congruence of the mating surfaces. Each meniscus is a crescent-shaped fibrocartilaginous plate, having a triangular shape in the cut. The thick edge of the menisci is turned outward and fused with the capsule, and the thinned edge is inside the joint. Top surface the meniscus is concave and corresponds to the surface of the condyles of the femur, and the lower one is almost flat, lying on the upper articular surface of the tibia.
Shape of the knee joint
In terms of shape and range of motion, the knee joint is a complex block-rotation joint.
In terms of the shape of the articular surfaces, the knee joint is a typical condyle.
It allows movement around two axes: frontal and vertical (longitudinal).
A) axis of motion
Movements in the knee joint are carried out around two axes:
frontal(flexion, extension)
vertical(rotation of the lower leg in a bent position of the knee joint).
B) Types of movement
1) bending
2) extension
3) rotation of the lower leg in a bent position
Flexion and extension occur around the frontal axis in the knee joint with a total range of motion of 140-150°. When flexed, the lower leg forms an angle of about 40 ° with the thigh. With this movement, relaxation of the collateral ligaments occurs. Flexion is inhibited mainly by the cruciate ligaments of the knee and the tendon of the quadriceps femoris. Due to the relaxation of the collateral ligaments during flexion in the knee joint, rotation around the vertical axis is possible. The total range of active rotation in the knee joint is on average 15°, passive - 30-35°. The cruciate ligaments inhibit and limit inward rotation, and when rotated outward, they relax, but this movement is limited by the tension of the collateral ligaments. During extension in the knee joint, the thigh and lower leg are located on the same line, and the cruciate and collateral ligaments are strongly stretched, and the condyles of the thigh rest firmly against the proximal epiphysis of the tibia. In this position, the lower leg and thigh form a fixed support. The menisci of the knee joint change their shape and position during movements. During flexion and extension, the condyles of the femur move along their upper surface, and during rotation of the meniscus, together with the femur, they slide along the articular surface of the tibia.
Capsule of the knee joint
The capsule of the knee joint is large, but in a significant part of it is thin.
The articular capsule is attached slightly away from the edges of the articular surfaces of the thigh, tibia and patella. Therefore, on the thigh it rises in front, bypassing the facies patellaris, goes between the condyles and epicondyles on the sides, leaving the latter outside the capsule, for attaching muscles and ligaments, and descends behind to the edges of the articular surfaces of the condyles. In addition, in front, the synovial membrane forms a large inversion, bursa suprapatellaris, extending high between the femur and the quadriceps femoris. Sometimes the bursa suprapatellaris can be closed and isolated from the cavity of the knee joint. On the tibia, the capsule is attached along the edge of the articular surfaces of the condyles. On the patella, it adheres to the edges of its cartilaginous surface, as a result of which it appears to be inserted into the anterior part of the capsule, as if into a frame. On the sides of the joint are collateral ligaments running perpendicular to the frontal axis: on the medial side, lig. collaterale tibiale (from the epicondylus medialis of the thigh to the edge of the tibiae, growing together with the capsule and the medial meniscus), and from the lateral side, lig. collaterale fibulare (from epicondylus lateralis to the head of fibulae). On the back side of the capsule of the knee joint there are two ligaments that are woven into the back wall of the capsule - lig. popliteum arcuatum and lig. popliteum obliquum (one of the 3 end bundles of the m. semimembranosi tendon).
Bundles
Ligaments are dense formations of connective tissue that are necessary for fixing the ends of bones to each other. Near each knee joint, in the lateral sections, are the medial and lateral collateral ligaments. They additionally strengthen the joint capsule, limiting lateral movements in the knee joint.
Inside the knee joint between the articular surfaces of the femur and tibia are stretched anterior and posterior cruciate ligament. These ligaments limit excessive movements of the articular surfaces of the bones in the anteroposterior direction. P  The anterior cruciate ligament keeps the tibia from slipping forward relative to the femur. The posterior cruciate ligament keeps the tibia from slipping backward relative to the femur.
The anterior cruciate ligament keeps the tibia from slipping forward relative to the femur. The posterior cruciate ligament keeps the tibia from slipping backward relative to the femur.
The cruciate ligaments provide control over the movements of the knee joint during forward and backward movements. All ligaments of the knee joint are very important structures that provide stability to the knee joint.
The two connective tissue structures of the knee joint, similar to ligaments, are called menisci. They are located between the femur and tibia. The menisci are sometimes referred to as the "cartilage" of the knee joint, but the structure of the menisci is different from that of the articular cartilage that covers the articular surfaces of the bones.
Meniscus function:
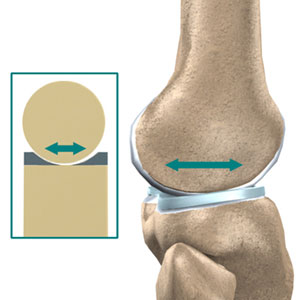
The biomechanics of the knee joint is easier to understand if you imagine this joint as a ball located on a flat area. The ball is the articular end of the femur, and the flat area is the tibial plateau. The menisci are elastic pads and fill the space between the femoral condyles and the tibial plateau. They help rationally redistribute body weight from the femur to the tibia.
In the absence of menisci, the entire body weight would be distributed at one point of the tibial plateau. The menisci distribute weight over almost the entire area of the tibial plateau. This role of the menisci is very important as it helps to protect the articular cartilage from excessive stress. Damage or absence of the meniscus leads to an incorrect distribution of loads in the knee joint, which contributes to the development of degenerative changes in the articular cartilage.
In addition to protecting the articular cartilage, the menisci, together with the ligaments, contribute to the stability of the knee joint. The stability of the joint is provided by its "wedging" of the menisci, which have a wedge-shaped shape. The thickness of the menisci is greater on the periphery than in the central part. This geometry results in the formation of a shallow depression on the tibial plateau. Such a surface gives greater stability to the joint, and more effectively redistributes static and dynamic loads on the articular surface of the tibia.
Thus, the ligaments and menisci of the knee joint are extremely important structures that contribute to the stabilization of the joint. Recall that ligaments connect bones to each other. Without strong ligaments connecting the femur and tibia, the knee joint would be very loose. In the knee joint, unlike other joints of our body, the geometry of the articular surfaces of the bones that form it does not provide additional stability.
Knee-joint, right. Front view.
1-femur; 2-tendons of the quadriceps femoris (cut off); 3-medial wide muscle of the thigh (cut off); 4-patella; 5-medial patellar ligament; 6-tibial collateral ligament; 7-ligament of the patella; 8-tuberosity of the tibia; 9-interosseous membrane of the leg; 10-head of the fibula; 11-anterior ligament of the head of the fibula; 12-fibular collateral ligament; 13-lateral supporting ligament of the patella; 14-lateral wide thigh muscle (cut off).
Muscles acting on the joint
The muscles and their tendons that surround the knee joint come from both the thigh and the calf. Topographically, they can be divided into three groups. The anterior group includes flexor muscles: the quadriceps femoris. Medial
|
medial |
||
|
[edge] - medialis - the side lying closer to the median (central) plane, i.e. inner side. |
||
|
click for details.. |
||
the group consists of the muscles that bring the thigh: the tailor muscle (in relation to the thigh, it belongs to the anterior group), the thin muscle and the large adductor muscle. The posterior group includes the hip extensors: biceps hips, semitendinosus and semimembranosus muscles.
Quadriceps femoris- one of the most massive muscles of the human body. It is located on the front surface of the thigh and has four heads, which are considered as independent muscles: the rectus femoris, the lateral broad muscle, the medial broad muscle and the intermediate broad muscle.
Rectus femoris starts from the anterior inferior iliac spine, goes down the anterior surface of the thigh and in the lower third of the thigh connects with the rest of the heads of the quadriceps femoris. The rectus muscle is a strong hip flexor. With distal support, it flexes the pelvis in relation to the thigh. The place of origin of the three broad muscles of the thigh are the anterior, outer and inner surfaces of the femur. All four heads of the quadriceps muscle are attached to the patella. In addition, the vastus intermedius muscle is partially attached to the capsule of the knee joint, forming the so-called muscle of the knee joint. From the patella to the tuberosity of the tibia, there is a ligament of the patella, which is a continuation of the tendon of the quadriceps femoris, which is thus attached to this tuberosity. The quadriceps femoris is clearly visible under the skin, especially its medial and lateral wide heads. Attention is drawn to the fact that the medial wide muscle descends lower than the lateral one. The general direction of the fibers of the quadriceps muscle is such that its structure is somewhat feathery. If we draw the resultant of this muscle, we can see that in relation to it the fibers of the rectus femoris muscle diverge from top to bottom, while the fibers of the wide muscles of the thigh (medial and lateral) go from top to bottom and inward, i.e. towards the median plane hips. This structural feature of the quadriceps femoris muscle increases its lifting force. Observing the contraction of this muscle on a living person, one can see that at the first moment of movement the muscle pulls up patella and fixes it. When the muscle relaxes patella somewhat lowered, and it becomes possible to produce its displacement.
Function patella is closely related to the function of the quadriceps femoris, for which it is a sesamoid bone, which contributes to an increase in the lever of force of the quadriceps femoris and, consequently, an increase in its torque.
The function of the quadriceps femoris muscle is to extend the lower leg and flex the hip, which is most possible with a bent lower leg
Sartorius is the longest muscle in the human body. It starts from the anterior superior iliac spine, passes in front of the hip joint, downwards and medially, first along the anterior, and then along the inner surface of the thigh, bypasses knee-joint With inside and attaches to the tibial tuberosity.
The function of this muscle is that, being biarticular, it produces flexion of the thigh and flexion of the lower leg. Having a somewhat spiral course, the sartorius muscle not only flexes the thigh, but also supinates it. Bending the shin, she also penetrates it. This muscle is clearly visible under the skin throughout with a bent, abducted and supinated thigh, as well as with an extended leg in the form of a cord between the quadriceps femoris muscle on one side and the adductor muscles on the other. The sartorius muscle is well palpable in the upper thigh.
thin muscle starts from the lower branch of the pubic bone and, going down in the form of a rather thin muscle cord, is attached to the tuberosity of the tibia. Of all the adductor muscles, this is the only biarticular muscle. The function of the thin muscle is that, passing near the knee joint, somewhat behind and inside of its transverse axis, it leads the thigh and contributes to the flexion of the lower leg in the knee joint.
Adductor major muscle- the largest of the muscles that bring the thigh. It starts from the ischial tuberosity and the outer surface of the branch of the ischium, and is attached to the rough line of the thigh and the medial epicondyle of the femur.
The main function of the muscle is to adduct the thigh. In addition, it plays a large role as a muscle that extends the thigh or pelvis in relation to the thigh. This function of the muscle increases as the hip flexes, since in this case the resultant muscle moves posteriorly from the transverse axis of the hip joint, the arm of the force becomes larger and its moment of rotation together increases significantly. On the contrary, with the hip extended, the direction of the resultant of this muscle almost coincides with the transverse axis of the hip joint, as a result of which the moment of rotation with respect to this axis approaches zero.
At the point of attachment on the lower leg, three muscles converge: tailor, semitendinosus and thin, forming the so-called superficial crow's foot, in the area of \u200b\u200bwhich there is a well-defined synovial bag.
The muscles of the thigh directly under the inguinal ligament form the femoral triangle. His upper bound makes up the inguinal ligament, the inner one is the long adductor muscle of the thigh, and the outer one is the sartorius muscle. At the bottom of this triangle are two muscles: the iliopsoas and the pectineus. From top to bottom, the triangle passes into the anterior femoral groove, in which the vessels and nerves pass.
In the lower third of the thigh, between the broad inner thigh muscle and the large adductor muscle, a dense connective tissue plate is thrown, which turns the anterior femoral groove into the adductor canal. Through this channel, the vessels from the thigh pass into the popliteal fossa.
Biceps femoris located on the outer side of the back of the thigh. As the name itself shows, this muscle has two heads, of which the long one starts from the ischial tuberosity, and the short one - from the lower part of the rough line of the thigh and the lateral intermuscular septum. The biceps femoris, passing behind the transverse axis of the knee joint, is attached to the head of the fibula.
The function of the muscle is to extend the thigh, flex the lower leg and supinate it.
As the lower leg flexes, the tendon of this muscle moves backward, due to which its moment of rotation increases. In the area of popliteal fossa the biceps femoris muscle is well palpable from the outside.
Semitendinosus located on the inside of the back of the thigh. It has a common origin with the long head of the biceps femoris on the ischial tuberosity. The semitendinosus muscle runs about knee joint behind and inside and is attached to the tuberosity of the tibia, participating in the formation of the superficial goose foot.
The function of this muscle is to extend the hip, flex the lower leg and pronate it, which is most possible with the lower leg bent.
|
pronation |
||
|
( |
||
|
click for details.. |
||
semimembranosus muscle begins on the ischial tuberosity, passes to the lower leg and is attached to the subarticular edge of the medial condyle of the tibia. In addition, the tendon of this muscle gives branches to the oblique popliteal ligament and to the fascia of the popliteal muscle. Three bundles of tendons leading to the three named formations make up the so-called deep goose foot.
The function of the semimembranosus muscle is to extend the thigh and flex the lower leg. Like the previous muscle, it participates as the lower leg flexes in its pronation.
Triceps muscle of the leg located on the back of the leg and has three heads. Two of them make up the superficial part of this muscle and are called the gastrocnemius muscle, and the deep part forms the so-called soleus muscle. All three heads pass into one common, calcaneal (Achilles) tendon, which is attached to the tuber of the calcaneus. Starting point calf muscle are the medial and lateral condyles of the femur. Its medial head is better developed and descends somewhat lower than the lateral one. The function of these heads is twofold: flexion of the lower leg at the knee joint and flexion of the foot at the ankle joint.
The soleus muscle originates from the posterior surface of the upper third of the body of the tibia, as well as from the tendon arch located between the tibia and fibula. This muscle is located deeper and somewhat lower than the calf muscle. Passing behind the ankle and subtalar joints, the soleus muscle causes flexion of the foot. Triceps the lower leg is clearly visible under the skin and is easily palpable. The calcaneal tendon protrudes significantly posterior to the transverse axis of the ankle joint, due to which the triceps muscle of the leg has a large moment of rotation in relation to this axis.
The medial and lateral heads of the gastrocnemius muscle are involved in the formation of the popliteal fossa, which has the shape of a rhombus. Its boundaries are: above and outside - the biceps femoris, above and inside - the semimembranosus muscle, and below - two heads of the gastrocnemius muscle and plantar muscle. The bottom of the fossa is the femur and the capsule of the knee joint. Through the popliteal fossa pass the nerves and blood vessels that feed the lower leg and foot.
Hamstring- a short flat muscle, directly adjacent to the back of the knee joint. It starts from the lateral condyle of the thigh, below the gastrocnemius muscle, and the bag of the knee joint, goes down and inward and attaches to the tibia above the line of the soleus muscle.
The function of this muscle is that it contributes not only to flexion of the lower leg, but also to its pronation. Due to the fact that this muscle is partially attached to the capsule of the knee joint, it pulls it back as the lower leg flexes.
|
lateral |
||
|
click for details.. |
||
|
distal |
||||
|
[ex. end, phalanx] (distalis)- the end of the muscle or bone of the limb or the whole structure (phalanx, muscle) most distant from the body. |
||||
|
click for details.. |
||||
|
(pronatio: lat. prono, pronatum tilt forward) - rotational movement of a limb or part of it (for example, forearm, hand or foot) inward, i.e. this is the rotation of a human limb around its long axis so that its front surface is about ... |
||||
|
click for details.. |
||||
Leg muscles, right. Front view
Leg muscles, right. Front view.
1-patella; 2-ligament of the patella; 3-calf muscle (medial head); 4 soleus muscle; 5-anterior tibial muscle; 6-tendon of the long extensor muscle of the big toe; 7-tendon of the muscle - short extensor of the big toe; 8-muscle-short extensor of the toes; 9-tendon of the third peroneal muscle; 10-lower retinaculum of the tendons of the extensor muscles; 11-upper retainer of the tendons of the extensor muscles; 12-muscle-long extensor of the toes; 13-short peroneal muscle; 14-long macho-tibial muscle; 15th - dexterity of the fibula.
thigh muscles, right. Back view.
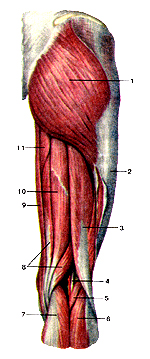
1-gluteus maximus muscle; 2-ilio-tibial tract; 3-biceps femoris; 4-nerve and blood vessels in the popliteal fossa; 5 plantar muscle; 6-calf muscle (lateral head); 7-calf muscle (medial head); 8-semimembranous muscle; 9-thin muscle; 10-semitendinosus muscle; 11-large adductor muscle.
Bibliography
Human anatomy: textbook. for stud. inst. physical cult. / Ed. Kozlova V.I. - M., "Physical culture and sport", 1978
Sapin M.R., Nikityuk D.K. Pocket atlas of human anatomy. M., Elista: APP "Dzhangar", 1999
Sapin M.R Human Anatomy
Sinelnikov R. D. Atlas of human anatomy: in 3 volumes. 3rd ed. M.: "Medicine", 1967
