
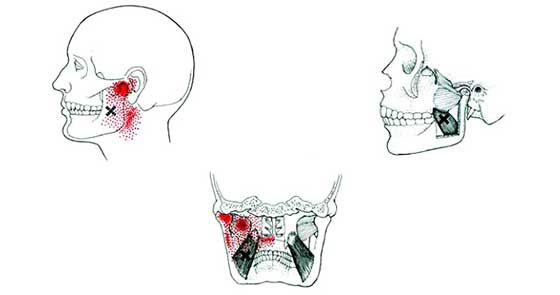
Pain and crunching in the jaw when chewing may indicate dysfunction of the temporomandibular lower jaw joint(TMJ). This is a functional pathology that affects 30 to 75% of dental patients, and is more common in young women.
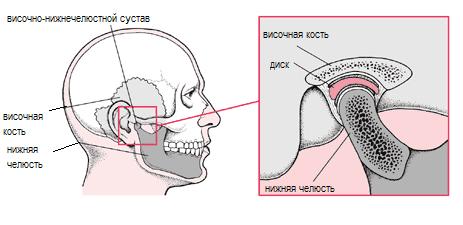
The temporomandibular joint takes on increased loads every day. He "works" almost continuously - when talking, eating, swallowing.
The jaw joint connects temporal bone and lower jaw, making it mobile. During normal operation of the TMJ, the lower jaw moves synchronously from the right and left sides.
However, various disorders of the skull, jaw muscles or elements of the joint itself lead to dysfunction of the entire masticatory apparatus and deterioration of its coordinated movements.
Causes of pain in the jaw joint
- Head or neck injuries such as severe bruises, which lead to displacement of the intra-articular cartilage disc;
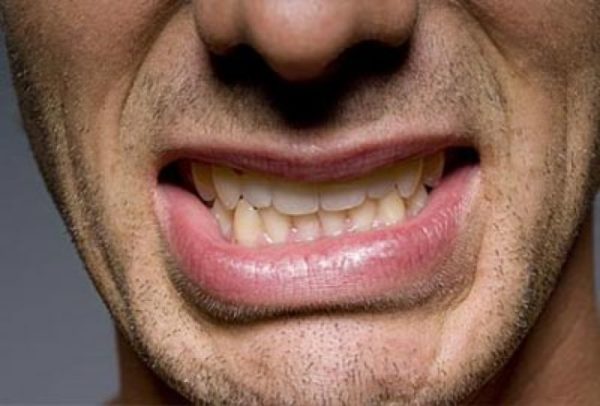
- bruxism - spontaneous nocturnal grinding of teeth;
- malocclusion or missing some teeth;
- low-quality dentures or too “high” fillings;
- one-sided type of chewing food;
- a state of stress in which a person strains the facial muscles and grits his teeth;
- rheumatoid arthritis, osteoarthritis and other diseases.
Dentist answers questions about TMJ
With diseases of the TMJ, you can feel that the jaw clicks or crackles when chewing. There is also an acute or It's a dull pain in the joint, which subsides over time or lasts for several years.
Other symptoms:
- pain in the facial area, near the neck or ear, which is aggravated by chewing;
- discomfort and difficulty opening the mouth;
- sharp blocking or clamping of the jaw in one position;
- overexertion of the facial muscles;
- a feeling of an “uncomfortable” bite, when the teeth on the upper and lower rows do not meet correctly;
- swelling of one side of the face.
At later stages there is headache and dizziness, tinnitus, discomfort in the shoulder area. Possible and concomitant symptoms like snoring, sleep disturbance, depression, difficulty in swallowing.
Diagnosis of TMJ dysfunctions
At the initial examination, the dentist finds out the patient's complaints and performs palpation in the joint area. It is also important to assess the amplitude (degree) of mouth opening. Devices are used to measure the nature of the work of the muscles of the head in different conditions.
As a rule, the diagnosis includes the removal of casts for the manufacture of plaster models of the jaw. This allows you to identify violations in the work of the jaw system, including incorrect occlusion (closing of teeth).
In some cases, computed tomography, MRI, as well as ultrasound of the jaw are prescribed.
It often happens that violations of the jaw joint are associated with unsuccessful prosthetics or complex extraction of teeth. Then pain dysfunction appears only 10-12 days after the procedure.
Consequences (complications) of TMJ dysfunction
Syndrome of dysfunction of the temporomandibular joint - most dangerous disease, which can eventually lead to ankylosis. It is stiffness or complete immobility mandible, which is accompanied by a violation of breathing, speech, as well as facial asymmetry.
In addition, it is possible dystrophic changes in the tissues of the joint, the development of arthrosis and other chronic ailments.
Therefore, do not postpone a visit to the dentist, the treatment of dysfunction of the temporomandibular joint is a must. The list of specialized specialists is presented below.
TMJ SYNDROME honey.
Temporomandibular joint syndrome - a symptom complex that manifests itself as pain on palpation chewing muscles, crackling during movements in the temporomandibular joint (TMJ) and / or pain above it with limited mobility of the lower jaw. The predominant age is 30-50 years. The predominant gender is female (3:1).
Etiology
Synovitis TMJTMJ disc pathology
Bruxism - teeth grinding during sleep
Spasm of chewing muscles
TMJ injury
Inadequate fitting of dentures.
Risk factors
The habit of clenching the jaw, grinding the teeth, yawning frequentlyOsteoarthritis, rheumatoid arthritis
malocclusion
Fibromyalgia
Psychosocial stress.
Pathomorphology
Displacement of the mandibular condyle head or anterior TMJ discTMJ capsulitis
Disc metaplasia leading to disc perforation and degeneration.
Clinical picture
Pain in the cheekbones and/or TMJLimitation of joint mobility
Clicking, grinding, crackling during movements in the TMJ
Headache
Pain in the ear canal
Irradiation of pain in the neck.
X-ray examination
Contrast video arthrography allows you to determine the degree of mobility of the TMJ and disc during chewing. MRI to assess disc positionArthroscopy for the purpose of visual examination of intra-articular structures.
Differential Diagnosis
Fracture or dislocation of the lower jawNeuralgia trigeminal nerve
Periodontitis
Neoplasms with lesions of the TMJ.
Treatment:
Conservative therapyRejection bad habits causing muscle tension and excessive TMJ mobility
Fixation of the lower jaw
Bite correction with orthodontic devices
Local physiotherapy procedures with thermal effect
Central muscle relaxants: mydocalm 0.05-0.1 g 2-3 r / day
NSAIDs: indomethacin 25 mg 3 r / day, voltaren 25 mg 3 r / day, etc. Periodic administration is recommended during treatment general analyzes blood, urine, FEGDS
To reduce pain.-.amit-riptyline 25 mg at night.
Surgical treatment should be used to correct a misaligned disc or replace a diseased disc if conservative therapy has failed.
Complications
Chronic dislocation of the TMJJoint contractures
Depression.
See also Arthritis, rheumatoid
Reduction. TMJ - temporomandibular joint
ICD
K07.6 Diseases of the temporomandibular jointDisease Handbook. 2012 .
See what "temporomandibular joint syndrome" is in other dictionaries:
FREY SYNDROME- (Lucy Frey syndrome, Bayarzhe syndrome; first described by the French doctor L. E. Dupuy, later by the French neurologist and psychiatrist J. G. F. Baillarge, 1815–1890, a detailed description was given by the Polish doctor Lucja Frey Gottesman, 1889–1942; synonyms - ... ...
Costen's syndrome- (J. B. Costen, born in 1896, American otorhinolaryngologist) a combination of pathological changes in the temporomandibular joint (clicking, crunching, stiffness), hearing loss, a feeling of stuffy ear, dull pains in the ear, radiating to the parietal ... Big Medical Dictionary
FACIAL PAIN- Common causes of facial pain are trigeminal neuralgia, temporomandibular joint syndrome, diseases of the teeth, paranasal sinuses, glaucoma. Trigeminal neuralgia is characterized by short (several seconds or minutes) ... ... Encyclopedic Dictionary of Psychology and Pedagogy
HEADACHE- - one of the most common complaints, often reflecting problems in the body as a whole. Headaches can be divided into primary and secondary. In primary headaches, the most thorough examination does not reveal any organic ... ... Encyclopedic Dictionary of Psychology and Pedagogy
Pathological tooth wear- This article has a list of sources or external links, but the sources of individual statements remain unclear due to the lack of footnotes ... Wikipedia
List of medical abbreviations- This page is a glossary. # A ... Wikipedia
Increased tooth wear- Pathological abrasion of teeth Pathological abrasion of teeth ICD 10 K03.0. Pathological abrasion of teeth is a pathology in which there is an intense loss of TV ... Wikipedia
Pathological anatomy of the jaw bones- The lesions of the jaw bones are varied. In the well-known guide to oncomorphology, published by the Institute of Pathology armed forces USA, in the volume on tumors and tumor-like processes of the jaw bones (2001), 71 diseases are described. ... ... Wikipedia
The condition of the temporomandibular joints (TMJ) prior to dental treatment will affect the outcome of complex dentures or orthodontic treatment. If the patient has problems with these joints, and this is not taken into account in the treatment plan, then even the best prostheses or implants will not bring maximum comfort to the patient. Why? This question is answered by the specialists of the clinic "Dial-Dent".
The main symptoms of TMJ dysfunction are:
- Pain syndrome: pain in the temples, neck, head (especially in the back of the head, often mistaken for a migraine); dizziness not associated with general physiological disorders of the body; pain localized in the face; pain of varying intensity when chewing.
- Clicking in the temporomandibular joints (when chewing, with a wide opening of the mouth, during yawning). This symptom may not bother the patient, but dentists should take it into account when prosthetics, as the problem can be aggravated by the appearance of pain. Sometimes clicks in the temporomandibular joints may appear several months after prosthetics, which means that the treatment was not performed satisfactorily.
- Inability to open the mouth wide.
- Hearing impairment not related to the state of the ENT organs, ringing or noise in the ears.
- Dysphagia or difficulty swallowing due to excessive muscle tension.
- Bruxism or grinding of teeth.
- Increased sensitivity of the teeth, exposure of the necks of the teeth are symptoms of excessive muscle tension in the dental system.
- Violations of posture, numbness of the fingertips - all these are symptoms of disorders in the cervical spine, one way or another associated with dysfunction of the temporomandibular joints.
- Snoring, short-term cessation of breathing during sleep, which occurs due to the backward displacement of the lower jaw. This is especially true when sleeping on your back.
If you observe three or more signs in yourself, then you need to consult a specialist to determine accurate diagnosis, it is likely that you have problems with the bite and the condition of the temporomandibular joints. You can get such a consultation at the Dial-Dent center.
TMJ dysfunction of varying degrees occurs in 25-50% of people of any age. This problem may be caused various reasons and has different manifestations and therefore difficult to diagnose. Patients with TMJ dysfunction turn to a neurologist, an otorhinolaryngologist, who do not help to cope with the problem. Most often, the symptoms of dysfunction of the jaw joints are associated with the state of the bite, teeth or dentures. Therefore, diagnosis and treatment should be carried out by a dentist who specializes in this field - this is usually a gnatologist or neuromuscular dentist. A neuromuscular dentist will determine what exactly it is connected with, and what specialists will help to cope with the disease: an orthopedic dentist, a neurologist, an osteopath, a psychologist, etc.
Prosthetics or implantation of teeth, as well as orthodontic treatment, should be carried out taking into account the diagnosis.
What causes TMJ dysfunction?
Pain is the main symptom of TMJ dysfunction that patients seek medical attention for. If you can still live with clicks in the joints or snoring, then it is impossible to ignore the pain for a long time. You can, of course, relieve the attack by taking painkillers, but the pain will return again. The principle of its appearance is with a constant spasm of the jaw muscles caused by various reasons. The main and most common cause of jaw joint dysfunction is stress. According to statistics, up to 80% of people react to stress with muscle tension. Most often, the muscles of the face, dentoalveolar apparatus, the back of the head, neck, and shoulders are clamped. Constant stress leads to muscle spasms that do not go away on their own, which causes pain.
Another cause of TMJ dysfunction is posture problems with insufficient physical activity. The balance of the muscles of the back and neck is disturbed, in which the jaw joints suffer. The jaw joints can be compared to the "princess and the pea" - as soon as the work of some part of the spine is slightly shifted (constantly carrying a bag on one shoulder, working in uncomfortable conditions, the so-called "office syndrome"), the jaw joints stop working correctly.
Inadequate prosthetics or missing teeth, especially chewing teeth, can provoke TMJ problems. All this leads to a violation of the correct closing of the teeth and, as a result, to the incorrect operation of the TMJ. Upper airway disorders can also cause similar conditions.
Neuromuscular diagnostics in Dial-Dent
For diagnostics, special devices are used that measure the status muscular system heads and necks, which determine the ideal position of the bite, in which the correct functioning of the jaw joints is restored. A number of tests are performed to establish the nature of muscle work in different conditions. The diagnostics also includes a traditional dental examination with x-rays, making dental casts, CT scan examining the patient's posture. The psychological and emotional state of the patient is taken into account.
The neuromuscular dentist determines the ideal position of the lower jaw (i.e. bite) based on the correct interaction of teeth, facial muscles and temporal joints. As a result, the doctor establishes a neuromuscular bite (neuromuscular occlusion), which may differ from the usual bite.
Habitual bite is not always correct
Until recently, it was believed that the natural closing of the teeth is correct position teeth. In many cases, this statement is true, since the body adapts to non-ideal conditions, compensating for certain violations. But there are cases when prosthetics in the usual bite does not become satisfactory for the patient.
That is why a multidisciplinary approach is important before complex dental treatment: it is necessary to establish the perfect bite, and only then begin planning, prosthetics, implantation or orthodontic treatment. This is the only way to get an excellent treatment result that justifies the time and financial costs of the patient.
Treatment tactics for TMJ dysfunction in Dial-Dent
- Helping patients to reduce stress levels, correct lifestyle problems, advice on exercise, massage. The patient's awareness of excessive muscle tension associated with increased stress, relaxation techniques and special exercises will help to cope with recurrent pain in the jaw joints. Specialists: psychologist S.V. Gornov, child psychologist T.B. Zukor, osteopath A.I. Popov.
- Dental treatment aimed at establishing the correct occlusion of the teeth by grinding the protruding parts of the teeth that interfere with proper contact. Specialists: treatment by the dentists of the clinic after consultation with the neuromuscular dentist A.V. Galeeva.
- Preliminary treatment with a removable splint "Orthotic" (orthotic). Orthotic is used to place the jaw in neuromuscular occlusion. The splint is put on the lower teeth, modeling the correct bite. Orthotic is worn according to the scheme prescribed by the doctor (usually 3-6 months) and in most cases leads to the disappearance of pain symptoms. Sometimes wearing an orthotic can cause a temporary deterioration in the condition (inability to chew, pain, etc.). This is due to the fact that the body has adapted to the wrong conditions and it takes time to return to the correct state. It is for this that the orthotic is used - for the gradual restoration of the correct bite. In some cases, the pathology is so strong that the reverse adaptation does not occur. Symptoms remain or go away slowly, and further treatment will be so difficult that the patient is not ready to continue it. In this case, part of the costs spent on treatment can be returned by the clinic. Specialists: neuromuscular dentist A.V. Galeev, orthopedist S.V. Zukor (complex dental treatment).
- Comprehensive difficult treatment after wearing an orthotic. At positive results after wearing the orthotic, the patient can undergo further treatment: either complete prosthetics (orthodontic treatment) in the correct bite, or keep the orthotic permanently worn. Rejection complex treatment and the removal of the orthotic will lead to the return of the old bite and joint problems. Specialists: neuromuscular dentist A.V. Galeev, orthopedist S.V. Zukor (complex dental treatment), orthodontist O.A. Baranova (complex orthodontic treatment).
- Referral to other specialists in case of diagnosing conditions associated not only with the pathology of the dentoalveolar system: a strong stressful condition, which requires the intervention of a neuropsychiatrist; arthrosis or arthritis of the joint, displacement of the intra-articular disc, which may require surgical intervention.
Comprehensive treatment of dental problems guarantees a stable positive result!
In this article, you will learn all about the diagnosis of temporomandibular joint dysfunction. About what are conservative methods treatments, splints, medicines and gymnastics. Special attention will be given to varieties surgical operations on the . We will also consider the possible causes of the disease and its prevention.
Symptoms
Temporomandibular cartilage dysfunction can have a large and varied number of manifestations. Discomfort affects not only the joint itself. It goes into the ear, occipital, facial region. Teeth begin to suffer. There are no nerves in the cartilaginous layers themselves, so they do not hurt by themselves. However, pain extends far beyond this articular connection.

Jaw dysfunction syndrome has the following symptoms:
- The joints of the jaw click, and it is not always painful. The sound is heard not only in the head of the patient, it is sometimes heard by other people. With such clicks, internal displacement of the joint is already present. So, there are also spasmodic muscle contractions. They are transmitted in the front and cervical region spine.
- Blocked . The jaw moves unevenly due to the changes that have happened inside. The patient understands that the jaw opens unevenly. In order to fully push the jaws, you need to develop the lower one a little, moving it in different directions. Often the joint begins to function normally only at the moment when an unpleasant clicking is heard.
- The joint is close to the organs of hearing. And if there are problems with the cartilaginous surfaces, the ear starts to hurt. It lays, there are problems with hearing, it rings, it makes noise in the ears.
- Headache. Heavy pressure on temples, occipital region. Sometimes there is a feeling that shoulder girdle put pressure weight. Doctors may confuse these symptoms with migraines or high blood pressure.
- The man starts grinding his teeth. This phenomenon is called bruxism. As a result, the muscles and the head begin to hurt even more. Bruxism harms, among other things, the teeth.
- Enamel sensitivity is manifested, sometimes because of this, teeth are even removed without finding the real reason.
- All of these symptoms lead to insomnia. But even during the day, a person does not begin to feel good. Sometimes there are mental problems: depressive states, anxiety.

The reasons
Bruxism is not only a symptom, but also a cause of dysfunction temporomandibular joint. Constantly grinding our teeth, strongly squeezing them, we injure the jaw cartilage.
Another reason is arthritis, that is, inflammation of the joint. May occur against the background of a weakened immune system. The infectious agent enters the body and affects the jaw joint. Cartilaginous tissues are destroyed due to the inflammatory process, their normal performance decreases.
Also, dysfunction of the jaw joint can develop as a result of mechanical damage. Especially if the first health care and subsequent treatment were not provided correctly, not fast enough.
Negative symptoms in this area can cause:
- neuralgic disorders of the facial nerves;
- inflammatory processes and hematomas, for example, after surgical operations;
- the appearance and subsequent growth of wisdom teeth;
- inflammatory process salivary glands;
- muscle disease and intervertebral discs neck;
- malocclusion.

Who is affected?
The following populations are affected by maxillofacial joint dysfunction:
- Children. Concentrate several risk factors. They often fall, their teeth grow. Kids today are under a lot of stress. Because of the pressure to study, the classes, the expectations of the parents, the child may begin to suffer from bruxism.
- Boxers and athletes in other areas of martial arts. In the ring, an athlete receives many blows every day, including in the face and jaw. Over time, these disruptions can lead to negative consequences, articular surfaces will be violated.
- Experiencing constant stress. This includes businessmen, people of intense intellectual work, students in the session. Incessant tension leads to the fact that a person squeezes and erases his teeth against each other.
- Working in bad conditions, at low temperatures. The cold can adversely affect the joints by weakening the immune system. As a result, an infection enters the cartilage tissue, arthritis begins. Its consequence is unpleasant clicks of the jaw joint.

Prevention
Preventive measures include:
- treatment of malocclusion;
- timely and high-quality made dentures;
- timely performed, adequate assistance for facial injuries;
- treatment of depression, negative psychological conditions;
- timely elimination of stress factors and situations.
A separate place in the prevention of mandibular syndrome is the treatment of bruxism:
- a hot bath before a night's rest;
- periodic use of a compress from a fabric soaked in warm water on the lower jaw;
- a minimum of stressful and emotionally negative states;
- volitional control over your jaws during wakefulness and falling asleep, do not close them;
- before going to bed, calm down, read something, listen to light tunes;
- the last meal of the day should consist of strong fruits, for example, apples, which will make the jaws tired;
- exclusion of tea, coffee and burning food in the afternoon.
Treatment

We offer the following medical methods for jaw dysfunction:
- Eliminate muscle spasm by applying warm, moist compresses.
- Visit a dentist to start treating your bite. You will have to spend two years with braces, but the effects will have a good effect not only on appearance, but also on health.
- Visit a psychologist to understand the causes of your psychological stress. A competent psychologist can teach you methods for relaxation.

Muscle relaxant Sirdalud price 350 rubles
To relieve unpleasant symptoms, the following medications will be required:
- Painkillers. Useful for migraines, pain in the face.
- Non-steroidal anti-inflammatory. Used to relieve inflammation inside the jaw joints. They also help to stop pain and some spasms. But these funds have a negative impact on digestive system, and you need to choose the minimum dosage for yourself.
- Muscle relaxants. These drugs are effective for relieving muscle spasms (for example, Sirdalud). However, they can be used only if there is no exacerbation of the inflammatory process. You need to drink muscle relaxants only in courses, otherwise there will be no positive effect. You also need to be careful with the dosage, one of the probable side effects is confusion and disorientation.
- vascular drugs. They will help if as a result of the combination cervical osteochondrosis and dysfunction of the joint, the blood circulation of the brain worsened.
Diagnostics
In the case of dysfunction of the jaw joint, it is quite difficult to carry it out. First of all, it is required to find out the causes that caused the disease.
The patient requires the following diagnostic procedures:
- collecting an anamnesis, studying what the patient complains about;
- study of the function of the head and;
- examination by a neurologist;
- x-ray of the lower part of the skull;
- cephalometry;
- occlusography.

A whole block of diagnostics is occupied by dental examinations:
- taking dental impressions;
- creating a model for diagnostics;
- specific mouthguards to check for bruxism;
- evaluation of bite functionality;
- condition of contacts between teeth.
All these levels of research are needed to correctly confirm the diagnosis. It is necessary for adequate treatment of dysfunction of the temporomandibular joint.
Splints for teeth
A splint worn over the teeth effectively relaxes the jaw joint. It does not allow him to make unnecessary movements, is the best prevention of night attacks of bruxism.
A soft splint is usually made from silicone materials individually to the shape of the patient's bite. Muscles relax, disappear muscle spasms. At first, there may be slight discomfort, but after a maximum of a week, all patients get used to it. These orthopedic products are worn comfortably and require minimal maintenance.

Sometimes soft tires are supplemented with a rigid frame for fixation. They work more effectively, but are less comfortable to wear.
Jaw gymnastics
The best treatment for joints is therapeutic exercises:
- Put thumb below the chin. Open your mouth against finger pressure.
- Place your thumbs at the bottom of the jaw, grab your chin with your index fingers. As you close your jaw, apply pressure with all your fingers.
- Put your tongue on the sky. Gently move your jaw up and down.
- Squeeze the pencil with your cutters. Move your jawbone left and right.
- Without removing the pencil from your mouth, move your jaw forward relative to your upper incisors. Return to normal position and then forward again.
Operations
In advanced cases of jaw damage, the following operations may be required:
- Minimally invasive surgery. The surgeon anesthetizes the patient and cleans the jaw joint. Small scars disappear, the inflammatory process stops. The joint is cleared of microscopic pieces of destroyed cartilage tissue. Better joint fluid is produced, which ensures the elasticity of cartilage.
- Arthroscopy. If the joint is blocked, the joined cartilage adhesions will need to be removed with a small scalpel. For this, tiny, almost imperceptible incisions are used.
- Open surgery. Applies only if no other methods already work. The incisions are quite large, through which the replacement of deformed tissues is carried out. For these purposes, healthy cartilage tissues of the patient himself are usually used.
Video "Dysfunction of the masticatory joint"
This video tells all about jaw dysfunction.
Temporomandibular joint dysfunction syndrome is one of the most difficult and controversial diagnoses that practicing dentists have to deal with. About 57% of patients seeking help from a dentist have some kind of complaint about dysfunction of the temporomandibular joint. From 14% to 29% of children and adolescents suffer from this disease. Diversity clinical manifestations dysfunction of the temporomandibular joint is determined by the polyetiology (multiple determining factors) of the pathological changes developing in it, which complicates the diagnosis and treatment.
most common cause development of dysfunction of the TMJ joints is - stress.
No less common causes of TMJ dysfunction are the mistakes of dentists of all specialties and/or non-compliance by patients with the recommendations of specialists. For example, improper placement of a filling on a chewing tooth can break the symmetry in the work of the TMJ joints, lead to unilateral overloads, then displacement of the discs, and finally, to the syndrome of TMJ joint dysfunction.
To others possible reasons diseases include:
- joint injuries
- long-term receptions at the dentist without rest breaks (3 or more hours)
- decrease in bite height due to loss of teeth and their increased abrasion
- bruxism (involuntary clenching and grinding of teeth)
- excessive exercise during sports
- taking some hormonal contraceptives!
- malocclusionand many other reasons...
Since dysfunction of the TMJ joints is difficult to treat, and many dentists do not have sufficient training to help such patients, patients do not receive the required timely assistance and go from one doctor to another, and not only dentists, but also therapists, otolaryngologists, neuropathologists and other professionals. Some specialists prefer to avoid such patients, since many of them already have pronounced changes in the joint that are not amenable to conservative correction. In the US and Europe, the cost of treating temporomandibular joint dysfunction is in second place, second only to therapy. malignant tumors. This indicates the high urgency of this problem.Since there are many different symptoms TMJ lesions, it is difficult to make a proper diagnosis.
Clicks and other noises in the temporomandibular joint.
The most common symptom of a TMJ lesion is clicking in the joint of the lower jaw. These sounds can be so loud that others can hear them when you chew, yawn, or simply open your mouth. Joint pain may or may not be present. But one thing is for sure: if the disc is displaced (and it usually is) when clicking occurs, then the muscles that move the lower jaw during chewing are more tense than normal. This tension leads to pain in the muscles, face, head and neck.
Headache
Headache is one of the most common symptoms of TMJ pathology. Usually, a headache in the pathology of the TMJ is located in the temples, the back of the head, and even the shoulders (shoulder blades). Jaw clenching and teeth grinding can be symptoms of TMJ pathology; these symptoms cause muscle pain, which can be the cause of headaches. A displaced TMJ disc can also cause joint pain that often radiates to the temples, forehead, or neck. These headaches are often so severe that doctors take them and treat them (without much success) as migraines or brain disorders.
Blocking (capture, locking) of the TMJ.
E This term is used to refer to uneven movement in the joint, due to violations in it. TMJ blockage can be seen simply as uneven movement when opening the lower jaw (as if it is catching something). Sometimes a person with a blocked joint must move the lower jaw from one side to the other in order to open the mouth wide. It also happens that a person has to open his mouth until he hears and / or feels a loud sound at the point where the lower jaw actually “unlocks”.
Change in bite
Abnormalities in the TMJ can also be manifested by changes in dental occlusion, or bite. If the TMJ disc is misaligned, then the bones and disc do not fit together properly and therefore the bite of the teeth changes.
Ear symptoms.
Due to the proximity of the TMJ to auricles, TMJ involvement often causes a variety of ear symptoms. Some of the symptoms are ear pain, stuffiness or dullness, up to and including hearing loss. That is why many patients with TMJ lesions first turn to their local doctor and ENT specialist.
Increased tooth sensitivity.
If the TMJ disc is misaligned, the teeth can become very sensitive, in part due to movements such as clenching and grinding of the teeth. Patients often go to their dentist complaining of pain in their teeth, but the doctor cannot always find the cause of this pain. Unfortunately, unnecessary procedures are often performed - depulpation of teeth, and even tooth extractions when trying to help a suffering person.
Inflammatory symptoms arthritis or synovitis in the joint cannot be confused with anything. Patients always complain of pain in the joint, swelling of the soft tissues around it, fever, general weakness and malaise.
Other symptoms.
Many other symptoms can be associated with TMJ pathology. Often there is pain in the shoulders (shoulder blades) and back due to increased tension (spasm) of the muscles, dizziness, sleep disturbance and appetite. Depression is often observed in the pathology of the TMJ. It may be due to the patient's experience of the fact that no one can understand the problem that causes such pain and suffering. In addition, a lot of scientific evidence shows that patients with chronic pain (and almost all patients with TMJ pathology are like that) have changes in their chemical structures brain.
Treatment.
Treatment always begins with a diagnosis.
Diagnosis is complex, complex,long and multi-day process. For starters, do functional diagnostics, to identify the causes of the pathology. It includes a whole range of procedures - identifying complaints, collecting medical data, examining the muscles of the head and neck, neurological examination, X-ray diagnostics (cone beam and magnetic resonance imaging, lateral teleroentgenography), cephalometric analysis, occlusography, detection of parafunctions and others. There are small and large functional analysis.
At the stage of small dental functional analysis, primary diagnostics are carried out, impressions are taken, diagnostic models are made, special mouthguards are made for examination for bruxism, bite, quality of interdental contacts, etc. are assessed. Large functional analysis is the most difficult to implement and interpret data and requires special knowledge, skills and equipment.
These functional tests are essential for making a correct diagnosis, and a correct diagnosis, in turn, allows for adequate therapy. Depending on the data obtained, the treatment can be conservative, reconstructive and surgical.
Conservative treatment includes - pain relief, swelling, making a mouthguard or joint splint. Further dynamic observation and, if necessary, reconstructive treatment.
Reconstructive treatment is usuallynot in the acute phase and is associated with a change in the position of the articular head of the condyle of the lower jaw and can be carried out according to different technologies. In this case, it is possible to change not only the position of the condyle, but also to correct the position of the articular disc, deprogramming of the muscular-ligamentous apparatus, and normalization of occlusion.
These tasks are performed by an orthopedist in a team with an orthodontist, periodontist, therapist and surgeon. Those. complex interdisciplinary approach. In some cases, consultation with a neurologist, ENT doctor, psychotherapist, osteopath, etc. is required. Often it is required to perform a complete reconstruction of the dentition with crowns, inlays, onlays with or without orthodontic preparation.
Surgical treatment consists of arthroplasty and is carried out in specialized surgical centers. It is used in the most difficult cases,unresponsive to other treatments.
M.L. Kasperovich,
dentist,
Candidate of Medical Sciences
