The radius is part of the forearm and consists of several parts that can be damaged. According to statistics styloid fracture radius accounts for about half of all damage. Often the damage is combined with an injury to the radius in a typical location. In order for this type of fracture to occur, there must be specific causes that should be dealt with in more detail.
The capsule is inserted medially at the top edge articular surface elbow joint, and in the lateral direction - on the upper edge of the ulnar notch of the radius. The synovial membrane covers the entire deep face of the joint capsule and, proximally, leaves a notch between the ulna and the radius, called the saccoid notch.
There are two ligaments that stabilize it: anterior and posterior radar vines. The first goes from the ulnar notch of the radius to the head ulna on its front surface; the posterior side is directed to the same level, but posteriorly from the ulnar notch of the radius to the ulnar soloid.
First of all, it is necessary to look at the position in which the person falls. Most often, this can happen when falling on an outstretched arm, a person instinctively stretches it forward. This feature is the most common cause damage. In some cases, a fracture of the styloid process of the radius is the result of a direct blow to the bone. In the latter situation, the fracture is often open, there is a wound of various sizes.
People who often train on a bike have injuries upper limb which are very different from other sports. Usually not traumatic injuries occur as a result of overload, which may or may not be accompanied by inadequate technique. We are talking about chronic injuries.
Anatomical revision of the upper limb
Very often, these traumatic injuries occur due to poor or incorrect adaptation to the bike. In the hand, we highlight three areas with 27 bones: carp, metacarpus and fingers. There are 2 bones on the forearm and humerus 1 is the humerus. The anatomical description of muscles, tendons, ligaments, arteries, veins, and nerves is quite complex, so we won't delve deeper than what the images can provide.

The frequency of such damage increases sharply in winter. On the ice, the elderly become especially vulnerable, an additional factor is osteoporosis. Injury can also occur when:
- passion for cycling, roller skating, skateboarding;
- professional sports;
- unsuccessful jump;
- active games.
Falls in such conditions contribute to the fact that the victim at the level of instinct stretches his arm forward and this leads to serious damage to the styloid process. In view of this, in addition to open or closed fracture, you can meet compression or tear damage.
People who frequently train on a bicycle have upper limb injuries that are very different from other sports where injuries predominate, such as epicondylitis, rotator cuff tensinopathy, or others. This is manifested as a result of compression of the median nerve. It can even appear as a result of a small microtrauma at the same level with peripheral inflammation and nerve irritation. Similarly, if the hand is placed in upper part rudder, with carp at maximum stretch, excessive lengthening of the nerve will be produced, which also causes irritation.
 In the photo, such an injury is a small crack. The mechanism of damage is associated with the impact of a nearby area of the wrist on the styloid process, as a result, due to the force of the impact, the radial process is repelled with force outward and somewhat backward. Often, the impact force is transmitted through the adjacent navicular bone, which can also be damaged.
In the photo, such an injury is a small crack. The mechanism of damage is associated with the impact of a nearby area of the wrist on the styloid process, as a result, due to the force of the impact, the radial process is repelled with force outward and somewhat backward. Often, the impact force is transmitted through the adjacent navicular bone, which can also be damaged.
As a consequence, the symptoms that appear are associated with changes in fine motor activity, hypoesthesia and paresthesia. thumb, index, middle and half of the ring. This situation is described by patients as "oily fingers" as they are prone to falling objects due to the lack of reinforcing force. In the study, we usually find a positive Phalen maneuver and an equally positive Tinel sign.
This symptomatology usually occurs only with sports practice and disappears outside the sports field. In these cases, the use of analgesics is usually not indicated. In the beginning, we can use preparations of B vitamins, since they reduce irritation of the nerves.
Symptoms of damage
A person is worried about several characteristic symptoms at once, all of them with additional methods surveys allow us to put an end to the question. The clinic is represented by:
- pain at the site of injury;
- crunch of fragments, which is called "crepitus";
- due to pain of movement wrist joint sharply limited;
- the fracture site is edematous;
- a hematoma forms under the skin;
- as the hematoma grows, there is a feeling of skin tension in the joint area.
The last symptom is not characteristic and is not determined in all cases.
In this case, the affected nerve is the motor branch of the ulnar nerve. The mechanism is usually the same as in the case of carpal tunnel syndrome, microtrauma, or continuous compression at the level of the Guyon canal with nerve irritation. This compression of the ulnar nerve occurs when hand device is located at the top of the rudder with the maximum elongation of the carp. The symptomatology that appears is also hypoesthesia and paresthesia, even with loss of strength in the fifth and fourth fingers. Watemberg and Frament's sign usually appears.
As a treatment, it is important to change the position of the hand and wrist on the steering wheel and avoid vibration at the same level. It might be interesting to fit wider wheels, reduce the number of wheels, and use padded gloves. Quanver tendinitis - inflammation of the long abductor and short extensor of the thumb, at the level of the styloid process of the radius. This usually results from wrist support on handlebars with cubital deviation. Due to this change in position at the level of the rudder, an angular relationship of the aforementioned tendons occurs.
Diagnostics
Before taking any action to treat or eliminate the bias, it is necessary to establish an accurate diagnosis. Initially, an x-ray must be taken and always in two projections. If in doubt, CT is indicated; if cartilage damage is suspected, MRI is indicated.

Tenosynovitis of the radial extensors and extensors of the fingers
In fact, inflammation occurs at the level of the fibrous-bone tunnel, which is called tendosynovitis. At the radial level of styloids, there is strong pain. As a treatment, we will use the orthosis throughout the day, even when you are cycling. When it is a chronic process, the use of acupuncture along with homoetic medicines and bioregulators are usually very effective. This injury occurs in those cyclists or triathletes who train or compete for long distances and the road surface is irregular, paved or paved.
Immediately after the injury, a cold object or ice, previously wrapped in a cloth, should be applied to the injury site. The cold will help reduce pain and reduce tissue swelling. The duration is from 15 to 20 minutes, after which a break is taken and the procedure is repeated several times. The limb must be immobilized with a special splint or any available means.
By exercising in this type of surface the athlete gains a stronger handle, after the forearm the musculature is overloaded, causing hypertrophy of the short and long adductor extensor muscles of the thumb, extending above the radial dilators, which they are compressed against deep planes.
Usually there is continuous pain in the movements of stretching the flexion of the wrist, sometimes even a slight crepitus is heard. It will be necessary to change the training routes with another type of asphalt, more regular. In the anatomical position, as well as the ulna and the medial side is the radio. Formed by the ulna and radius bones, interconnected by an interosseous membrane. In addition to the joint with the elbow, the forearm has two proper movements, and supination. Movement in elbow joint carried out with the help of the brachioradialis muscle. The bone is long, parallel and lateral to the ulna. The shaft has three ribs and three faces Interosseous edge dorsal front edge previous edge of the face dorsal surface of the lateral surface The radio receiver articulates with four bones: humerus, ulnar, scaphoid and crescent-shaped. It articulates proximally: Along the concavity of the head of the radius, with the head of the humerus. the circumference of the head of the radio joint articulates with the radial notch of the ulna. It articulates distally: from the carpal bones of the face through the carpal joint and the ulna through the ulnar incision. The most distal end is from the styloid process and the distal side. long bones, parallel and occupy the medial side of the forearm. proximal epiphysis olecranon - great elevation forming the tip of the elbow. Block groove - a large depression formed in the process of the olecranon and coronoid process and serves for articulation with the shoulder block. Distal epiphysis The head of the ulnar - articular Elevation of the round is located in the lateral direction. styloid process - located more medially and more prominent. The shaft has three ribs and three face Facets of the interosseous dorsal front edge previous edge of the face dorsal front face The ulna articulates with two bones: the humerus and the radio. articulates proximally: block of the humerus with block incision. with the radio through a radial groove in which the circumference of the head of the radius rotates and articulates distally: Down side The head of the ulna articulates with the articular disc, which separates the carpal bones. May be required surgery if weakened or unstable cartilage fragments. Which of the two bones of the forearm is located laterally, given the anatomical position? What is the joint structure that maintains the relationship between radius and ulna found in the body of both bones? What is the executable movement at the forearm joints? What is the name of the eminence located medially in the radius where the biceps tendon joins? Does the carpal articular facet of the radius articulate with the carpal bones? How many and what are the bones with which the radius articulates? Which bone of the forearm articulates with humerus? What is the name given to the bones of the accident commonly called the tip of the elbow? Is that a forearm bone? What is the purpose of this structure? How many and what are the bones with which the elbow joint articulates? What is the relationship between the notches and the heads of the radius and ulna? The radial mark is located proximally, and the ulnar notch is located distally. Is this statement correct? How many and which elbow joints? The umeroradial joint is of the ginglymoid type and the radioulnar joint is of the trochoid type. Consists of two bones parallel to each other. . Treatment of fractures of the distal third of the radius with external fixation and bone graft.
 In the trauma center, the doctor performs the reposition of the fracture. For this, a special manipulation is performed, the control of which is carried out using an x-ray. The process of repositioning fragments is carried out under local or general anesthesia depending on the complexity of the fracture. The doctor's hand is on inside wrist joint, the second pulls the limb towards itself. After that, the brush is retracted to the elbow side and plaster is applied. If the compression force is insufficient, then there is a risk of re-displacement.
In the trauma center, the doctor performs the reposition of the fracture. For this, a special manipulation is performed, the control of which is carried out using an x-ray. The process of repositioning fragments is carried out under local or general anesthesia depending on the complexity of the fracture. The doctor's hand is on inside wrist joint, the second pulls the limb towards itself. After that, the brush is retracted to the elbow side and plaster is applied. If the compression force is insufficient, then there is a risk of re-displacement.
The author presents a prospective study using an external fixation technique associated with autogenous bone graft for the treatment of distal radius articular and metaphysical fractures. 36 patients were treated, mean age 52.2 years. Follow-up had a mean time of 36.2 months. The stability of the reduction and its maintenance were guaranteed by external fixation using an autogenous bone graft. In patients undergoing bone densitometric analysis, the presence of an autologous graft is statistically stable over time.
Avulsion type fracture of the styloid process of the radius
This type of damage is not as common as previously described. The cause of an avulsion fracture is the tension of the radial collateral ligament, as a result of which the site of its attachment is damaged. A similar type of damage can occur after a person falls on an outstretched arm, there is a subluxation of the wrist joint inwards. At this point, the wrist is displaced inward, at which point a radius fracture may occur in a typical location, but the styloid process is torn off.
It would be possible to revive rehabilitation in this method and, in favor of mobilization, start in the next postoperative period. In the fourth week, the external fixation device is removed, allowing free movement of the wrist, less strain, which is prevented by a dorsal "orthosis" for two additional weeks. The analysis of data obtained as a result of treatment is considered an anatomical and functional aspect. Anatomical data were obtained from radiographic studies of patients. Their analysis was based on the Sheck method and was considered excellent in 72% of patients, while good in 28% was satisfactory in their integrity.
Symptoms
Immediately after an injury, a person is disturbed characteristic symptoms. According to their complex, an avulsion fracture of the styloid process of the ulna can be diagnosed. Characteristic is:
- severe pain at the site of injury;
- increased pain when trying to move;
- the area of the wrist joint is deformed;
- crunch of fragments when trying to move;
- numbness of the fingers;
- increased pain when tapping on the base of the palm;
- the pain is aggravated when walking or during movement of the upper limb.
 Knowledge of the anamnesis, the nature of the injury and a simple medical examination is sometimes not enough to make a correct diagnosis. To make a correct diagnosis, it is necessary to perform an x-ray, always in two projections. If the doctor has doubts on the x-ray, a CT scan is indicated.
Knowledge of the anamnesis, the nature of the injury and a simple medical examination is sometimes not enough to make a correct diagnosis. To make a correct diagnosis, it is necessary to perform an x-ray, always in two projections. If the doctor has doubts on the x-ray, a CT scan is indicated.
At week 24, 14% were considered unsatisfactory and 86% were satisfactory. The presence of pseudoarthrosis of the styloid process of the ulna was also detected in 33.3% of patients, which, however, developed in all cases without symptoms. Among the fractures that occur in the upper extremity, the distal radius is the most common and is estimated to represent 16% of all skeletal fractures.
Today, a distal radius fracture is viewed as a complex lesion with a variable prognosis depending on the type of treatment taken. This can be divided into conservative or non-surgical methods, as well as surgical restoration. AT conservative methods some degree of deviation in fracture alignment is accepted, emphasizing the functional outcome. The importance of the anatomical result is emphasized, comparing it with the functional result.
Treatment of an avulsion fracture
The subtleties of first aid and the reduction of displaced fragments have already been described above. With such an injury, plaster is applied for about a month with mandatory X-ray control 3-5 days and two weeks after the injury. When the fracture line passes through the articular surface of the radius, it is shown surgical treatment. The operation option is chosen by the doctor depending on the degree of displacement and the presence of fragments. Fixation is carried out with screws or with a plate.

Regardless of whether without mixing or with a displacement of the fracture, recommendations on nutrition and medication are relevant. The diet should be dominated by foods containing calcium, chonroitin and hyaluronic acid. Similar substances are found in:
- cottage cheese;
- sour cream;
- milk;
- aspic;
- gelatin products;
- hard cheeses;
- seafood.
Additionally, the body needs protein, its source is meat. Useful for the body will be low-fat varieties of veal, rabbit, poultry. You can supplement the diet with legumes, herbs, dried apricots, figs. The source of vitamin D for humans is fish fat.
Helps accelerate fracture healing medical preparations. In particular, calcium preparations, especially in combination with vitamin D, for example, Calcium D3 Nycomed. Also used drugs: "Struktum", "Osteogenon", "Calcemin". Such funds are prescribed for the entire duration of treatment until the fracture is completely healed.
If there is severe pain, NSAIDs or non-steroidal anti-inflammatory drugs are used. Doctors use funds: "Ketorol", "Ketanov", "Revmoxicam", "Aertal", which can be used in the form of injections or tablets. The funds are used in short courses, with long-term use they can provoke the development of stomach ulcers.
A fracture is exactly the factor that triggers the mechanism for the onset of swelling. To prevent this complication, special decongestants are used. Preference is given to drugs: "Cyclo3 Fort", "Serrata". In addition, cold is applied to the plaster cast, as has already been described for its use at the first aid stage.
The appointment of chondroprotectors, agents that contribute to the restoration of articular cartilage, is shown. The course is three months, after which a break is made for a month and the course of treatment is repeated again. The drugs have one nice feature, which is that after their cancellation, the action continues. Means are used: "Hialual", "Protecon", "Chondroitin complex".
Recovery

Rehabilitation begins immediately after the application of a plaster splint. In the early period of rehabilitation, finger movements are shown. This will avoid stiff fingers and develop the muscles of the forearm. Despite the plaster cast, the appointment of physiotherapy procedures is indicated. In this period are shown: magnetotherapy and UHF, which improve blood flow and activate bone cells.
After four weeks, the plaster is removed after X-ray control. During this period, the range of rehabilitation opportunities expands significantly. For the first time after removing the plaster bandage, it is indicated to wear an orthosis. The appointment of therapeutic exercises, which is performed under the supervision of an exercise therapy instructor, is shown. Flexion and extension in the wrist joint, abduction and adduction of the hand are performed. After are added circular motions.
 Gymnastics is initially performed without load, which is gradually added as recovery progresses. As a load, it is recommended to use a regular sponge, which is compressed and unclenched. As training progresses, the arm is developed using a manual expander, it may have varying degrees rigidity.
Gymnastics is initially performed without load, which is gradually added as recovery progresses. As a load, it is recommended to use a regular sponge, which is compressed and unclenched. As training progresses, the arm is developed using a manual expander, it may have varying degrees rigidity.
Massage can speed up recovery after a fracture, which is also carried out under the supervision of an experienced specialist. Also, massage will lead to muscle tone, reduce tissue swelling, and improve blood flow.
Physiotherapy is shown, the list of which is expanding significantly. Shown:
- magnetotherapy;
- diodynamic;
- shock wave therapy;
- ultrasound.
Pain relief gels help to reduce pain during the recovery phase. You can apply them several times during the day on washed skin. Can be used: "Ketorol gel", "Diklak gel", "Flamydez gel", "Voltaren", etc.
Complications can be divided into early and late, depending on the time of occurrence. The early ones include:
- Purulent-septic complications (with open fracture).
- Secondary displacement (if the plaster is removed early).
- Vascular disorders at the site of injury.

To late complications worth considering:
- neurotrophic disorders.
- Deformities of bones and articular surface after fracture union.
- Post-traumatic deforming osteoarthritis.
When fragments of a fracture are set incorrectly or out of time, the joint is able to deform, the styloid process protrudes under the skin. In some situations, after an injury, a person is worried about pain at the fracture site.
Incorrectly fused fractures are not always corrected even with the help of surgery. In order to prevent a similar situation from happening again, after receiving an injury, a person should seek medical care see a traumatologist for an examination. A condition for the occurrence of complications is the early removal of gypsum, after which the fragments are displaced.
Comparison of fragments can be done under local anesthesia. For this purpose, 10-15 ml of a 2% solution of novocaine is injected into the fracture area along the dorsum of the forearm. It is also necessary to inject 2-3 ml of a 2% solution of novocaine into the fracture area of the styloid fragment, which doctors often do not do. Reposition of fragments should be started only after complete anesthesia in the area of the fracture occurs, therefore, after the introduction of novocaine solution, it is necessary to wait a few minutes. Usually, with the onset of anesthesia, patients improve their mood, the suffering expression on their faces disappears, and they allow you to touch your hand without fear.
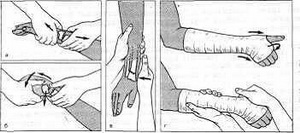
Reposition of fragments can be done both with the help of various devices and manually. For reduction by manual means, it is necessary to have two assistants. You can limit yourself to one, if in the office where the fragments are repositioned, there is a special device for fixing the shoulder and providing countertraction. The design of this device is simple, and it can be done in any trauma room. In one of the walls, several rings are strengthened at different distances from the floor in order to use them with different heights of the victims. A strong cord is attached to the ring, at the end of which there is a wide loop of durable fabric. The arm of the victim is passed through this loop and placed on the distal part of the shoulder. In order to make it convenient to put the loop on the injured arm, it can be cut and fastened with several buckles on the shoulder. When using the loop, there is no need for a second assistant (see Fig. 37).
After anesthesia, the victim is put on a bench and his arm is bent at the elbow joint at a right angle. If there is no special device, then one of the assistants sits on a chair opposite the patient, grabs with both hands and holds his shoulder. Another assistant with the right hand captures the area of elevation of the 1st finger, with the left - the rest of the fingers in case of damage right hand and, conversely, with the left hand - the area of \u200b\u200bthe first finger and with the right - the remaining fingers in case of a fracture of the left hand. Slowly, smoothly, without jerks, he produces a stretch in order to stretch the retracted muscles well enough. The surgeon stands with his back to the face of the victim and with the palm of one hand presses on the distal fragment from the radial side, and with the palm of the other produces counterpressure on the proximal fragment, eliminating the radial displacement of the distal fragment. At this time, the assistant, producing stretching for the hand, gives it the position of ulnar deviation. Having eliminated the lateral displacement, the surgeon positions his hands so that the first fingers of both hands are on the back, and the remaining fingers are on the palmar surface of the forearm. Having captured the distal part of the forearm in this way, the surgeon rests his fingers against the distal fragment displaced to the rear, while simultaneously shifting the proximal fragment to the rear with the remaining fingers of both hands (Fig. 40). Having eliminated this shift, two plaster splints are applied - the back wide and the palmar narrow, after which x-rays are taken in two projections.

Rice. 40. Reposition of fragments in a fracture of the radius in a typical location.
As already noted, accurate matching of fragments is important for restoring hand function. This can be established not only visually. One of the objective signs of standing fragments is the position of the radioulnar angle. Normally, it is defined as follows. On the radiograph, a vertical line is drawn through the radioulnar joint parallel to the longitudinal axis of the radius, perpendicular to it through the same joint - a horizontal line towards the apex of the styloid process of the radius. The angle formed by the third line and the horizontal line is radioulnar, which is normally 30° (Fig. 41). It must be remembered that the angle of inclination of the articular surface of the radius is normally 10 °. This angle is checked on a picture taken in a strictly profile position. Restoration of ratios is the main task in the reposition of fragments. A decrease or increase in angular ratios adversely affects the function of the bone.
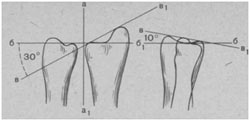
Rice. 41. Radioulnar angle in an intact wrist joint. Explanation in the text.
After the reposition of the fragments, a plaster cast is applied, and there is no need to fix the elbow joint. The plaster bandage should capture the forearm from the elbow to the metacarpophalangeal joints. The assistant holds the hand in the position of ulnar deviation and in a position intermediate between pronation and supination. We do not consider it necessary to give the hand an average physiological position. Dorsal or palmar flexion of the hand is determined by the direction of the break line. With a strictly transverse fracture line, the brush is given an average physiological position. If the fracture line runs obliquely in a distal direction from the back to the palmar side, the hand should be placed in a dorsiflexion position in which the distal fragment is well held. With an oblique fracture line running in the proximal direction from the back to the palmar side, the distal fragment is better held with palmar flexion of the hand.
Fixation can be ensured by a properly applied deep back plaster splint reinforced with a soft bandage. Some surgeons strengthen the splint with cast bandages, thereby turning it into a circular bandage, others fix the limb with the help of the dorsal and palmar plaster splints, which are strengthened with soft bandages. We do not attach great importance to the design of the cast, but we believe that each cast should fix the fragments well and not have constrictions and dents that cause discomfort.
After the bandage has hardened, the patient can be released home. The next day, he must come to the doctor to check the condition of the bandage. If the bandage compresses the forearm and causes circulatory disorders, then cut through the soft bandage that fixes the splint, loosen its edges a little and bandage it again. The circular bandage is dissected on the palmar side and slightly moved apart, after which it is fixed with a soft bandage. If the bandage weakens in the first days due to the disappearance of edema, then it, without removing the old bandages, is strengthened with new ones. After 5-7 days after applying the bandage, it is necessary to make a control radiograph, since after the edema subsides, a second displacement of the fragments may occur. Unfortunately, not all surgeons fulfill this requirement, so often after removing the bandage, incorrect fusion of the fragments is revealed. If a secondary displacement is detected, it is necessary to immediately reposition the fragments.
With fractures of the radius in a typical place without displacement the hands are given an average physiological position and a posterior plaster splint is applied from the upper third of the forearm to the metacarpophalangeal joints. From the first days after the reposition of fragments and the imposition of a plaster cast, the patient is recommended to make movements with the fingers and in the elbow joint, which contribute to better blood circulation, reduce swelling of the fingers and quickly restore their functions.
If the fragments were well matched and tightly held by a plaster bandage, then it can be removed after 4-5 weeks. By this time, fusion occurs, which is quite well expressed clinically and radiologically. If the fracture is not complicated, then the functions of the hand and forearm are usually restored by the 6-8th week.
After removing the bandage, a massage of the hand and forearm is prescribed, physiotherapy exercises to restore mobility in the wrist joint and in the joints of the fingers. Massage and gymnastics contribute to the disappearance of edema of the forearm and hand and stiffness of the fingers.
With an isolated fracture of the styloid process of the ulna impose a back gypsum splint from the middle third of the forearm to the metacarpophalangeal joints. The hand should be given an average physiological position and ulnar deviation. The plaster bandage is removed after 2-2 weeks. By this time, the work capacity of the victim is restored. If the separation of the styloid process is recognized in a timely manner and a plaster splint is immediately applied, then the damage usually disappears without a trace.
In case of marginal fractures of the radius, the fragments should be repositioned and the forearm fixed with a dorsal plaster splint for up to 3 weeks. Due to the fact that these fractures are intra-articular, their exact comparison is important in order to avoid a violation of the congruence of the wrist joint and the subsequent formation of deforming arthrosis with all the ensuing consequences.
Particularly difficult is treatment of comminuted comminuted fractures of the radius in a typical location. These fractures, as a rule, are intra-articular, and it is not easy to compare fragments of the epimetaphysis, broken into several parts, with each other, and then with the proximal fragment. In addition, if you manage to compare these fragments, then it is quite difficult to keep them in the right position. That is why the functional prognosis for such fractures is not very favorable. After fractures, mobility restrictions remain in the wrist joint and almost constant pain when moving due to a violation of the congruence of the joint.
Conservative treatment of such injuries is carried out in the same way as for non-comminuted fractures of the radius in a typical location. In most cases, it gives disappointing results. After local anesthesia, the fragments are repositioned manually or with the help of an apparatus. By squeezing the crushed metaepiphysis in the lateral and anteroposterior direction, they try to bring the fragments closer together. Then a plaster cast is applied, most often a circular one. In order to prevent secondary displacement of fragments under a plaster cast, L. Bohler (1928) proposed to pass one needle through II, III, IV and V metacarpal bones, and the other through the ulna in its upper third. Then I apply a circular plaster cast from the middle third of the shoulder to the metacarpophalangeal joints, gypsuming both needles and bending the forearm at the elbow joint at a right angle. With this method of treatment, the plaster cast is removed no earlier than after 6 weeks. After that, control x-rays are taken, the needles are removed and massage, therapeutic exercises and physiotherapy are prescribed.
V. A. Chernavsky (1947) offers a more active tactic for comminuted and tending to secondary displacements of fractures of the radius in a typical location. It lies in the fact that after comparing the fragments and X-ray control in a closed way through the distal fragment, several spokes are passed in different directions, which are determined by the X-ray. The spokes are carried out in such a way as to hold the fragments compared with each other and the entire metaepiphysis with the proximal part of the radius. With certain indications, such tactics are quite justified.
Dubrov Ya.G. Outpatient traumatology, 1986
