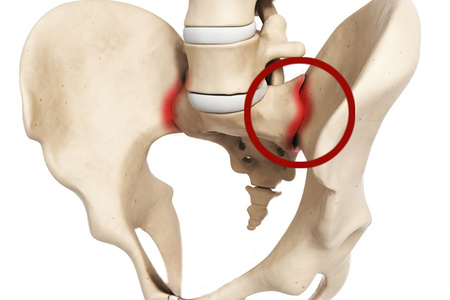
Pain in the sacroiliac joint often occurs when lifting heavy objects in an awkward position, when there is tension in the joint, supporting ligaments and soft tissues. Sacroiliac (the joint is also susceptible to the development of arthritis with various diseases, damaging articular cartilage. Osteoarthritis is a common form of arthritis that leads to pain in the sacroiliac joint: rheumatoid and post-traumatic arthritis are also common causes of pain. Less common reasons ankylosing spondylitis, infections and Lyme disease. Collagen diseases are more polyarthropathy than monoarthropathy limited to the sacroiliac joint, although SI joint pain from ankylosing spondylitis responds extremely well to the intra-articular injections described below. Sometimes patients experience iatrogenic dysfunction of the sacroiliac joint caused by traumatic bone graft removal.
Symptoms of pain in the sacroiliac joint
Most patients with sacroiliac joint pain complain of pain around the joint and in the upper leg that radiates to the buttock area and down the back of the leg; the pain never extends below the knee. Movement increases the pain, while rest and warmth bring relief. The pain is constant and can interfere with sleep. The affected sacroiliac joint is painful on palpation. Patients often spare the affected leg and lean toward the unaffected side. There is often spasm of the lumbar axial muscles, which limits movement in the lumbar spine in an extended position, and improves the necessary relaxation of the hamstrings in a sitting position. In patients with sacroiliac joint pain, the pelvic rocking test is positive. For this test, examiners place their hands on the iliac crests and thumbs on the anterior superior iliac spines and then with force brings the wings of the pelvis to the midline. A positive test is characterized by pain in the sacroiliac joint.
Clinical features of pain in the sacroiliac joint
Lesions of the sacroiliac joint from other injuries lumbar region the spine can be demarcated by asking the patient to lean forward in a sitting position. Patients with sacroiliac pain do this relatively easily due to the relaxation of the biceps femoris muscle in this position. In contrast, patients with low back pain experience increased symptoms when bending forward while sitting.
The injection described is quite effective in treating pain in the sacroiliac joint. Co-existing bursitis and tendinitis can increase pain in the sacroiliac joint, which requires additional treatment more local injections of local anesthetics and methylprednisilone.
An injection into the sacroiliac joint is carried out in a lying position, the skin over the joint is treated with an antiseptic solution. A sterile syringe containing 4 ml of 0.25% preservative-free bupivacaine and 40 mg methylprednisolone is connected to the needle in a sterile manner. Find the posterior superior spine ilium. At this point, the needle is carefully advanced through the skin and subcutaneous tissue at an angle of 45 degrees in the direction of the affected joint. If it hits the bone, the needle is withdrawn into the subcutaneous tissue and again directed higher and slightly laterally. After penetration into the joint, the contents of the syringe are carefully injected. There should be little resistance to injection. If significant resistance is observed, the needle has probably hit the ligament and should be advanced slightly into the articular area until the injection comes without significant resistance. Then the needle is removed, a sterile bandage and cold are applied to the injection site.
Physical therapy, including heat treatments and light exercises, should begin a few days after the injection. Excessive exercise should be avoided as it will worsen symptoms.
Survey
Plain radiography is indicated for all patients with pain in the sacroiliac joint. Since the sacrum is susceptible to traumatic fractures and the development of both primary and secondary tumors, MRI of the distal lumbar spine and sacrum is indicated if the cause of pain is unclear. In such patients, it is possible to conduct a radionuclide bone study (scintigraphy) to exclude tumors and incomplete fractures, which can be missed with conventional radiography. Based on clinical manifestations, additional tests can be performed, which include general analysis blood, ESR, determination of HLA B-27 antigen, antinuclear antibodies and blood biochemistry
Differential diagnosis
Pain originating from the sacroiliac joint can be mistaken for myogenic pain, lumbar bursitis, inflammatory arthritis and lumbar lesions spinal cord, roots, plexuses and nerves.
Treatment of pain in the sacroiliac joint
Initial treatment of SI joint pain and dysfunction includes a combination of NSAIDs (eg, diclofenac or lornoxicam) and physical therapy. Local application of heat and cold may also be helpful. For patients who do not respond to this treatment, injection of local anesthetics and steroids is indicated as a next step.
The sacroiliac joint is the main joint connecting the lower spine and the pelvis. It bears a huge load that occurs when moving the human torso.
Structure of the sacroiliac joint
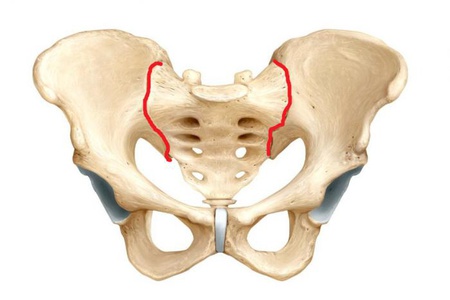
It is formed by fairly extensive articular surfaces of the sacrum and ilium of the pelvis. More precisely, this joint is located between the wedge-shaped “body” of the sacrum and the inner surface of the ilium.
From an anatomical point of view, such a structure refers to tight or inactive joints of the skeleton. It is paired and flat in shape.
Components of a joint
There is cartilage on both articular surfaces. However, its appearance is different for each of them. The iliac surface bears fibrous and thin cartilage. And the sacral one is hyaline and thicker.
If we consider this joint from above, then the upper third of it can be called a fibrous joint (syndesmosis). At the same time articular surfaces connected to each other by connective tissue. And only the lower two thirds are a typical joint. However, there is practically no joint space in it.
The joint capsule is a tightly stretched dense fibrous “bag”.
The sacroiliac joint is securely fixed by several ligaments, which have perhaps the strongest structure in the entire human body.
Ligamentous apparatus
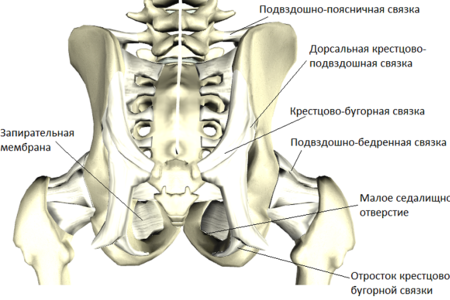
Ligaments in structure are connective tissue fibers collected in bundles. They connect the component parts of the joint, further strengthening it.
The strengthening of the sacroiliac joint itself is formed by several groups of ligaments that are located in front and behind this joint. Both of these groups (ventral and dorsal, respectively) contain interosseous sacroiliac ligaments. They are short, connecting the sacral and iliac tuberosities. These are very strong ligaments that are rightly considered one of the most resistant to tearing.
Also in each group there are ventral and dorsal sacroiliac ligaments. They arise from the corresponding anterior or posterior part of the ilium from below and fan-shapedly stretch to the lateral edge of the sacrum.
Additional links
In the anatomy and function of this joint important role Several more ligaments play, which are not actually articular. These include:
- Sacrotuberous ligament. It is located between the ischial tuberosity of the pelvic bone of the same name and the sacrum.
- Sacrospinous ligament. Located from the spine of the ischium to the edge of the sacrum.
- Iliopsoas ligament. Directed from the transverse processes of the fourth and fifth lumbar vertebrae to the upper part of the ilium.
The above ligaments do not directly relate to the sacroiliac joint, and they serve to strengthen the pelvis with the spine. These ligaments indirectly fix the sacroiliac joint.
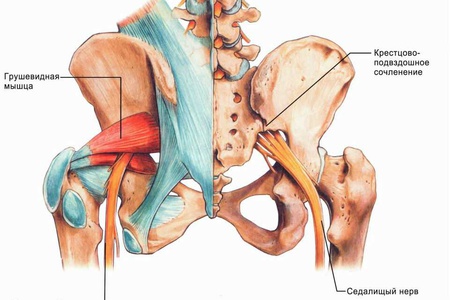
Blood supply and innervation
Blood enters and flows out to the sacroiliac joint through the vessels of the lumbar, iliopsoas and external sacral arteries and veins.
Innervation is carried out by branches of the lumbar and sacral nerve plexuses.
Function
The virtual absence of joint space, the system of powerful and short ligaments make active movements in the joint almost impossible. The range of movement usually does not exceed 4–5 degrees. However, in childhood or during pregnancy, the sacroiliac joint has more pronounced mobility.
The main function of this joint is to absorb movements transmitted from the lower extremities to the spine.
That is why it carries quite a significant static and dynamic load. Also, during childbirth in women, it, together with the pubic symphysis, increases the diameter of the birth canal (pelvis), facilitating the process of childbirth.
Joint pathology
For any disease of the sacroiliac joint, the main manifestation is pain. Painful sensations when this joint is damaged are quite characteristic. We will now look at these signs.
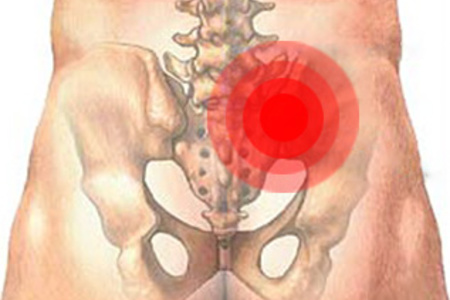
The pain is characterized as diffuse (spread out), without a clear source. It is determined by the outer part of the buttock. Spreads (irradiates) to the posterior surface of the corresponding lower limb to the knee hole. The pain can also sometimes spread to the groin area.
Pain increases noticeably with physical activity on the joint, for example, when running or standing on one leg.
Patients note that when moving sideways and in small steps, the pain noticeably decreases. Also, walking up the stairs is easier than going down.
Types of joint pathology
Pathological changes in this area can be caused by many factors. It is customary to divide all types of injuries to the sacrolumbar joint into several groups.
Traumatic injuries
Injuries to this joint in isolated form are very rare. They are usually combined with other injuries to the pelvis - for example, fractures of the pelvic bones or ruptures of the ligaments of the symphysis pubis. Such injuries usually appear as a result of various pelvic injuries (falls, road accidents, etc.), sometimes during complicated childbirth.
With such injuries, instability of the pelvic ring occurs, which is manifested by a displacement of the pelvic axis and the occurrence of damage (fracture, ligament rupture) in the sacroiliac joint.
Fractures
Fractures of the pelvic bones are very often accompanied by extensive internal bleeding with the formation of retroperitoneal hemorrhages, which is an extremely life-threatening condition. This requires emergency medical care.
The most pronounced manifestations of a fracture of the pelvic bones are:
- Pelvic deformity.
- Forced position of the lower limb with its outward rotation and disruption of its function.
- Intense pain at the sites of fractures, which increases noticeably when attempting to compress the pelvis.
Transportation of such patients should be done extremely carefully in a lying position on a backboard.
Sprains and ligament tears
Ligament ruptures are usually combined with damage to the ligamentous apparatus of the symphysis pubis. This complication sometimes occurs during childbirth during its pathological course. Diagnosis is usually carried out immediately and is confirmed by radiographic examination.
Sprains of this joint can occur during pregnancy and some time after childbirth.
The pain syndrome described above is characteristic. However, correct diagnosis is not always carried out, since in this group of patients it is impossible to carry out, for example, a pelvic x-ray.
Inflammatory diseases
Inflammatory lesions of the sacroiliac joint are called sacroiliitis. The main reasons that lead to the development of inflammation in the joint are:
- The action of pathogens of specific or nonspecific infection.
- Ankylosing spondylitis (Bechterew's disease).
- Other diseases accompanied by the development of joint inflammation (arthritis). This happens with rheumatoid or reactive arthritis, psoriasis, etc.
WITH detailed description manifestations of ankylosing spondylitis and other diseases in which inflammatory damage to the sacroiliac joint is only one of the symptoms can be found in the relevant sections of the site. As a rule, diagnosing these conditions does not present any particular difficulties.
Infectious lesion
The development of purulent sacroiliitis is caused by specific or nonspecific microflora. In the first case, inflammation appears when a person is infected with Treponema pallidum (the causative agent of syphilis), Mycobacterium tuberculosis, etc. These microorganisms cause quite specific, i.e., characteristic of a particular type of damage to cells and tissues.
Nonspecific microflora includes most pathogenic and conditionally pathogenic microorganisms (staphylococci, streptococci, anaerobes, etc.). Infection with several types of such microflora is usually encountered. Penetration of infection into the joint occurs in several ways:
- Hematogenous or with blood flow. Normally, there are no bacteria in the blood, that is, it is sterile. However, with some pathological conditions pathogenic microorganisms appear in it. This occurs, for example, with a significant decrease in immunity due to AIDS and other immunodeficiency conditions, the development of sepsis (blood poisoning), etc.
- Infection open wound. This happens when open fractures, significant bruises with massive hemorrhages (hematomas).
- Spread of purulent infection from nearby foci. For example, with purulent lesions of the pelvic bones or sacrum, the infection can mechanically penetrate into the sacroiliac joint. Thus, secondary infection occurs.
The course of sacroiliitis can be acute or subacute.
Acute sacroiliitis
The acute onset is manifested by an increase in body temperature to high numbers, symptoms of general intoxication - chills, weakness, headaches and muscle pain etc. Pain in the joint area is sometimes very intense, the patient is forced to be in a horizontal position. Moreover, lying on a completely flat surface (a shield) also causes significant pain.
A complication of the acute course of purulent sacroiliitis is often an abscess of the gluteal muscle.
In this case, the accumulated pus breaks through the joint capsule and pours into the surrounding tissues.
Subacute and chronic sacroiliitis
When a joint is affected by certain types of infectious agents, for example, brucellosis or tuberculosis, the course of the disease is not accompanied by such pronounced manifestations as in an acute process.
Body temperature may increase slightly or occasionally. There are no symptoms of intoxication or they are mild. Joint pain is usually of low intensity.
If this condition is untimely or insufficiently treated, it becomes chronic over time.
At the same time, pain in the lumbar region and sacrum often bothers you or even becomes constant. Spinal deformation may occur and the function of the lower limb may be impaired. There are signs in the joint itself chronic inflammation, which ultimately leads to its failure.
With, for example, tuberculosis of the joint, thigh abscesses often occur with the formation of fistulas.
Diagnosis of sacroiliitis
![]()
At acute course Diagnosis of the disease usually does not present any particular difficulties.
In subacute and chronic cases of sacroiliitis, special functional tests, radiography and MRI of the pelvis are often performed.
Osteoarthritis
Occurs as a result of non-infectious damage to the sacroiliac joint. In this condition, articular cartilage gradually deteriorates. As a result, over time, this leads to disruption of the normal functioning of the joint.
Osteoarthritis or osteoarthritis most often develops as a result of previous injury to the joint.
Also, such a pathology can develop after prolonged joint overload - playing sports, sedentary work, carrying heavy objects, pregnancy, etc.
The main manifestation of osteoarthritis is pain, which is constant or paroxysmal in nature. It intensifies with movements, prolonged standing, sitting, and bending forward. Localization pain located in the area of the sacrum or buttock with distribution to the lower back, thigh. Some stiffness may occur, often after a long period of rest or in the morning.
X-rays reveal osteophytes (bone growths), a decrease in the width of the joint space and other signs of osteoarthritis.
How to treat such a pathology?

Treatment of all diseases of the sacroiliac joint mainly depends on the cause that caused the pathological process in it:
- Traumatic lesions of the joint are usually combined with damage to other anatomical structures, such as the pelvis. Therefore, treatment of such injuries is carried out exclusively in a hospital setting, depending on the severity of the injuries.
- In treatment inflammatory diseases joint, it is very important to correctly determine the cause of the pathology. The principle of treatment of such conditions is etiological, affecting the cause of the disease. Thus, for infectious lesions, antibacterial drugs are primarily used.
- With intense pain syndrome Various painkillers and anti-inflammatory drugs are prescribed, as well as physiotherapy. If they are ineffective, blockades with the introduction of anesthetics are used. It's also possible intra-articular injection painkillers.
- Patients are limited in physical activity. Widely used various techniques manual therapy.
- Pregnant and postpartum women with damage to the sacroiliac joint are recommended to wear special bandages to unload the spine.
Sometimes shown surgical treatment. For example, when an abscess occurs due to purulent sacroiliitis.
How to forget about joint pain?
- Joint pain limits your movements and full life...
- You are worried about discomfort, crunching and systematic pain...
- You may have tried a bunch of medications, creams and ointments...
- But judging by the fact that you are reading these lines, they did not help you much...
But orthopedist Sergei Bubnovsky claims that indeed effective remedy for joint pain exists!
The support of our skeleton is made up of large bones located in different parts of the frame, such as the ilium, the largest of the pelvic bones. There are more than 200 different elements in the skeleton. Some are more durable, say, the bones that make up the skull, or the heel. Others are small and very fragile.
However, no matter how strong the bone tissue is, cases arise when even the strongest element is subject to destruction. The reasons are quite different:
- genetic predisposition;
- metabolic disorders;
- abrasion of the bone body with age or as a result of constant and prolonged physical activity;
- injuries with fractures and so on.
Fracture of the iliac bone - enough dangerous injury. Very severe, carries risk of major blood loss and damage internal organs, especially genitourinary.
Design features
This is a paired bone. Both elements (right and left) have the same anatomy. There are two main sections: the wing and the body.
The body is short and thick. Connecting with the pubic and ischial bones, the acetabulum is formed. The upper part of the bone element is expanded - this is the wing. It has an unusual structure. The very edge of the wing is slightly curved; this is a crest. At the anterior edge of the crest there is a pair of small outgrowths - the superior and inferior iliac spines. Below them is the large sciatic notch.
The inner and outer sides of the wing also have structural features:
- internal - forms the iliac fossa;
- outer – convex – gluteal surface.

The iliosacral junction of the pelvis is formed by the articulation of the inner surface of the wing by the auricular region with pelvic bone. The pubis, ischium and ilium together form pelvic bone. And in a pair they make up the pelvic girdle. The joints of the belt elements are very strong, formed due to the bone type of connective tissue.
Fractures of the pelvic bones occur only in 5-6% of cases. The main reason is compression of the pelvis due to an accident. As mentioned, the ilium breaks only in the most serious accidents or falls from a great height. The thinner pubic and ischial muscles are more often affected. And yet, even this large, strong bone element, which has such a seemingly monolithic structure, can be damaged.
Symptoms and treatment of a fracture
The most common cause of damage to these bones is fracture injuries. They are differentiated by severity. Therefore, an individual approach to treatment is required. Sometimes doctors resort to surgical intervention to help the patient regain his ability to work. In most cases, conservative therapy is sufficient.
It is known that the most dangerous are fractures with displacement, fragmentation type, open or in places of complicated reduction. When the ilium is damaged, the following symptoms are observed:
- unbearable, sharp pain, worsens when trying to move;
- extensive soft tissue hematoma;
- swelling;
- decreased functionality of the limb due to the injured bone element.
Regardless of the severity of the fracture and the location of the tissue rupture, the symptoms are similar. But the causes of injury vary.
- Direct blow or sharp cut gluteal muscles(in children) causes avulsions of the iliac spines.
- A fall from a height or an accident often affects the wing and ridge.
With such injuries, multiple ruptures of bone elements, that is, other bones of the pelvic girdle, are observed.

Closed reduction of fragments is performed under local anesthesia
At the slightest suspicion of a fracture, the victim should be immediately taken to a medical facility. Painkillers will help reduce pain. Unfortunately, traditional plaster immobilization is not applicable. The doctor administers anesthesia and then repositions the fragments:
- without displacement: local anesthesia, closed reduction;
- with offset: general anesthesia, open reduction (surgical method).
There is no fracture, but the bone “aches”?
There are other reasons why there is pain in the pelvic bones:
- tumor;
- blood diseases;
- excessive physical activity(professional);
- inflammation, infection;
- diseases associated with metabolic disorders in the bones;
- action medicines;
- congenital pathologies (disturbed anatomy);
- long bed rest;
- excessive secretion of certain substances;
- decrease in osteoblast activity (age-related);
- spinal osteochondrosis;
- intervertebral hernia.
Let's consider more detailed pathology associated with anatomical disorders.
The structure of bone is divided into periosteum, compact substance, spongy substance and bone marrow. Enostosis – pathological symptom, manifested by bone overgrowth from the inside bone tissue. The neoplasm may be small localized or spread throughout the entire length of the bone. This pathological change causes diffuse thickening of the cortex until the lumen of the medullary canal is completely closed. As a result, a person develops various diseases, the main symptom of which is enostosis.
By the way, enostosis can be detected intravitally only through x-ray examination, since the symptom has no external manifestations. The pathological process can begin in any bone of the skeleton, including the ilium.
The role of the iliac bones in medical research
Trephine biopsy allows obtaining samples bone marrow for a more detailed study of histology in order to confirm a particular pathological process. This technique is used directly when collecting material from the iliac bones.
Trephine biopsy is more productive than sternal puncture:
- causes less pain;
- less injuries;
- larger sample volume;
- the least disruption of the integrity of tissues and histological layers in the sample.
Trephine biopsy is performed in the crest area (from the side of the anterior superior or posterior tubercle). To extract the sample, a special trocar needle is used, first proposed by Professor Abramov.
Depending on the side of penetration, a different set of needles is used. Trephine biopsy requires precision and high professionalism of the doctor.
To ensure that the patient does not experience pain when the needle is inserted, anesthesia is performed. skin, subcutaneous tissue and periosteum. Then the doctor carefully inserts the trocar with the inserted mandrin, piercing the skin, subcutaneous tissue and approaching the surface of the bone.

Next, rotational movements are made with a special handle attached to the outer end of the trocar. The needle seems to be screwed in. The mandrin is removed, and the needle is screwed into the spongy substance until it stops. Without stopping rotation, the needle is slowly withdrawn. The collected sample is placed in a special saline solution. The puncture mark is disinfected with iodine and sealed with a band-aid.
Each element of our skeleton has its own role. And it is very important to ensure that they remain intact, strong and healthy. If pain occurs, do not hesitate to see a doctor. This way you can avoid serious problems in the future.
Pain from the sacroiliac joint often occurs when lifting heavy objects in an awkward position, or when there is tension in the joint, supporting ligaments and soft tissues.
The sacroiliac joint is also susceptible to the development of arthritis due to various diseases that damage the articular cartilage.
Osteoarthritis is a common form of arthritis that leads to pain in the sacroiliac joint: rheumatoid and post-traumatic arthritis are also common causes of pain.
Less common causes are ankylosing spondylitis, infections, etc.
Collagen diseases are more polyarthropathy than monoarthropathy limited to the sacroiliac joint, although SI joint pain from ankylosing spondylitis responds extremely well to the intra-articular injections described below.
Sometimes patients experience iatrogenic dysfunction of the sacroiliac joint caused by traumatic bone graft removal.
Symptoms
Most patients with sacroiliac joint pain complain of pain around the joint and in the upper leg that radiates to the buttock area and down the back of the leg; the pain never extends below the knee. Movement increases the pain, while rest and warmth bring relief. The pain is constant and can interfere with sleep.The affected sacroiliac joint is painful on palpation. Patients often spare the affected leg and lean toward the unaffected side. There is often spasm of the lumbar axial muscles, which limits movement in the lumbar spine in an extended position, and improves the necessary relaxation of the hamstrings in a sitting position. In patients with sacroiliac joint pain, the pelvic rocking test is positive.
For this test, the examiner places their hands on the iliac crests and thumbs on the anterior superior iliac spines and then forcefully brings the wings of the pelvis towards the midline. A positive test is characterized by pain in the sacroiliac joint.
Survey
Plain radiography is indicated for all patients with sacroiliac joint pain. Since the sacrum is susceptible to traumatic fractures and the development of both primary and secondary tumors, MRI of the distal lumbar spine and sacrum is indicated if the cause of pain is unclear.In such patients, it is possible to conduct a radionuclide bone study (scintigraphy) to exclude tumors and incomplete fractures, which can be missed with conventional radiography. Based on the clinical manifestations, additional tests can be performed, which include a complete blood count, ESR, determination of HLA B-27 antigen, antinuclear antibodies and blood biochemistry
Differential diagnosis
Pain originating from the sacroiliac joint can be mistaken for myogenic pain, lumbar bursitis, inflammatory arthritis, and lesions of the lumbar spinal cord, roots, plexuses, and nerves.Treatment
Initial treatment of SI joint pain and dysfunction includes a combination of NSAIDs (eg, diclofenac or lornoxicam) and physical therapy. Local application of heat and cold may also be helpful. For patients who do not respond to this treatment, injection of local anesthetics and steroids is indicated as a next step.Complications and diagnostic errors
The injection technique is safe with good knowledge of anatomy. For example, if the needle is inserted laterally, it may damage sciatic nerve. The main complication of intra-articular injection is infection, which, with strict adherence to asepsis and universal precautions, is extremely rare.The appearance of ecchymoses and the formation of hematomas can be reduced by compressing the injection site immediately after it is performed. Approximately 25% of patients complain of a transient increase in pain after intra-articular injection; they should be warned about this.
Clinical features
Sacroiliac joint injuries can be differentiated from other lumbar spine injuries by asking the patient to lean forward in a sitting position. Patients with sacroiliac pain do this relatively easily due to the relaxation of the biceps femoris muscle in this position. In contrast, patients with low back pain experience increased symptoms when bending forward while sitting.The injection described is quite effective in treating pain in the sacroiliac joint. Co-existing bursitis and tendonitis may increase SI joint pain, requiring additional treatment with more local injections of local anesthetic and methylprednisilone.
An injection into the sacroiliac joint is carried out in a lying position, the skin over the joint is treated with an antiseptic solution. A sterile syringe containing 4 ml of 0.25% preservative-free bupivacaine and 40 mg methylprednisolone is connected to the needle in a sterile manner.
The posterior superior iliac spine is located. At this point, the needle is carefully advanced through the skin and subcutaneous tissue at an angle of 45 degrees in the direction of the affected joint. If it enters the bone, the needle is withdrawn into the subcutaneous tissue and again directed higher and slightly laterally. After penetration into the joint, the contents of the syringe are carefully injected.
There should be little resistance to injection. If significant resistance is observed, the needle has probably entered the ligament and should be advanced slightly into the joint area until the injection comes without significant resistance. Then the needle is removed, a sterile bandage and cold are applied to the injection site.
Physical therapy, including heat treatments and light exercises, should begin a few days after the injection. Excessive exercise should be avoided as it will worsen symptoms.
R.G. Esin, O.R. Esin, G.D. Akhmadeeva, G.V. Salikhova
The ilium is one of the largest bones of the human skeleton. The right and left iliac bones are located in the superoposterior portions of the pelvic bone.
Structure of the ilium
The ilia are paired. Therefore, both the left and right iliac bones have the same structure. They have two parts: the body and the wing. The body is the short and thick section of the ilium. It fuses with the ischium and pubis bones, forming acetabulum. Extended upper part The ilium forms a wing. The curved upper edge of the wing is called the iliac crest. On the front of the crest there are two small outgrowths - the inferior and superior iliac spines. Somewhat below them is the greater sciatic notch. The inner concave part of the wing forms the iliac fossa, and the convex outer part forms the gluteal surface. On the inner surface of the ilium wing there is an auricular surface, which is the place of articulation of the sacrum and the pelvic bone.
Fracture of the ilium
Iliac fractures usually result from direct blow or compression of the pelvic bones. In children, a fracture in the area of the iliac wing can also occur as a result of a sharp contraction of the buttock muscles. Symptoms of a fracture are:
- Severe tissue swelling at the fracture site;
- Sharp pain that intensifies with any attempt to move the leg;
- A sharp decrease in the function of the lower limb on the affected side, i.e. In case of injury to the right iliac bone, functions are impaired right leg, and in case of damage to the left - accordingly to the left.
A fracture of the ilium is accompanied by significant hemorrhage, which spreads along the entire lateral surface of the pelvis and the upper third of the thigh. Tension of the muscles of the anterior abdominal wall is often observed.
If a fracture of the ilium is suspected, the victim should be taken to the hospital in a supine position. A small cushion is placed under the knees. If the fracture is not displaced, then local anesthesia is applied to the fracture area, the leg is placed in a special splint and strict bed rest is prescribed for three to four weeks. For displaced fractures, perform surgery, the purpose of which is to compare and fragments (reposition), after which the leg is placed in a splint and the injured patient is prescribed bed rest for a month. Then physiotherapeutic treatment and massage are prescribed. Classes are required physical therapy. Typically, complete restoration of lower limb function is observed 1.5 to 2 months after discontinuation of bed rest. 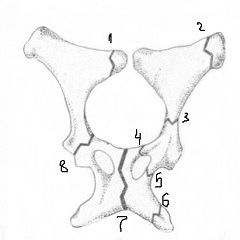
Ilium hurts: causes
In addition to injuries, there are other reasons why the ilium hurts. They are quite varied:
- High physical activity when playing sports;
- Tumors of the iliac bones;
- Blood diseases ( multiple myeloma, erythremia, chronic myeloid leukemia, acute, bone marrow diseases, Hodgkin lymphoma);
- Infectious lesions of the iliac bones (,);
- Metabolic bone diseases (mineral and/or vitamin D deficiency, osteomalacia, vitamin B1 deficiency);
- Excessive secretion of cortisol, T3 or parathyroid hormone;
- The effect of certain medications, in particular hormonal drugs;
- Prolonged stay on bed rest;
- Suppression of osteoblast activity caused by age;
- Congenital pathology of collagen synthesis (Paget's disease).
In addition, pain in the area of the right or left ilium can occur with herniated intervertebral discs. Therefore, if the ilium hurts, you should not self-medicate, but should consult a doctor. Only a doctor, having carried out all the necessary medical examination of the patient, will be able to find out the real reason pain, make a correct diagnosis and prescribe appropriate treatment.
Attention, TODAY only!
Everything interesting
Humerus- the skeletal basis of the shoulder, a long tubular bone. Structure of the humerus The humerus consists of a body and two epiphyses - the distal lower and proximal upper. In the lower part of the body of the bone there is a posterior surface,…
The metatarsus is the part of the foot between the tarsal bone and the phalanges of the toes. The metatarsus is formed by five tubular bones. Structure of the metatarsal bone Each metatarsal bone has a wedge-shaped base, a body and a head. The second metatarsal bone is the longest, and...
The ischium is one of three bones that, together with the ilium and pubis, form the pelvic bone. After 16-17 years, these bones are connected using cartilage, and later, after complete ossification of the cartilage, the boundaries between them are completely...
The pelvic bone is made up of three bones, and this includes the pubic bone. The paired pubic bone is composed of the body, as well as the upper and lower branches, they are located at an angle to each other. The two upper branches of the pubic bone are connected to each other...
Pathological bone fracture is a process that usually occurs as a result of a slight physiological load on a bone that has previously been subjected to some pathological phenomenon: inflammation, infectious process, dystrophic change And…
