Bones in the human body are not located in isolation from each other, but are interconnected into one single whole. Moreover, the nature of their connection is determined by functional conditions: in some parts of the skeleton, the movements between the bones are more pronounced, in others - less. More P.F. Leosgaft wrote that “in no other department of anatomy is it possible to so “smoothly” and consistently reveal the relationship between form and administration” (function). By the shape of the connecting bones, you can determine the nature of the movement, and by the nature of the movements, you can imagine the shape of the joints.
Hinged joints are classified functionally as multi-axial joints. The femur and humerus are able to move both in the anterior and medial-lateral directions, and can also rotate around their long axis. The shallow socket formed by the glenoid cavity allows the shoulder joint to use a wide range of motion. In contrast, the deep socket of the acetabulum and the strong supporting ligaments of the hip joint serve to limit hip movement, reflecting the need for stability and bearing capacity on the thigh.
The main position when connecting the bones is that they are “connected to each other in such a way that with the smallest volume of the junction there is the greatest variety and magnitude of movements with the greatest possible strength in the most advantageous opposition to the influence of shocks and concussions” (P.F. Lesgaft) .
The whole variety of bone connections can be represented as three main types. There are continuous connections - synarthrosis, discontinuous - diarthrosis and semi-discontinuous - hemiarthrosis (half-joints).
Watch this video to see the synovial joint animation in action. Synovial joints are places where bones articulate with each other within the joint cavity. The different types of synovial joints are swivel joint, articulation joint, articulation joint, condyloid joint, saddle joint and planar joint.
Which type of synovial joint allows the widest range of motion? Joints Arthritis is a common synovial joint disorder that involves inflammation of the joint. This often results in significant joint pain as well as swelling, stiffness, and reduced joint mobility. There are over 100 various forms arthritis. Arthritis can occur due to aging, damage to articular cartilage, autoimmune disease, bacterial or viral infections or unknown reasons.
Continuous connections bones are called those in which there is no break between the bones, they are connected by a continuous layer of tissue.
Intermittent connections- these are when there is a break between the connecting bones - a cavity.
Semi-discontinuous connections characterized by the fact that in the tissue, which is located between the connecting bones, there is a small cavity - a gap (2-3 mm), filled with liquid. However, this cavity does not completely separate the bones, and the main elements of the discontinuous connection are absent. An example of this type of connection is the connection between the pubic bones.
Risk factors that may lead to osteoarthritis later in life include joint damage; jobs associated with physical labor; sports with running, twisting or throwing actions; and overweight. These factors put stress on the articular cartilage that covers the surfaces of the bones at synovial joints, causing the cartilage to gradually become thinner. As the layer of articular cartilage wears out, there is more pressure on the bones. The joint responds to increased production of lubricating synovial fluid, but this can lead to swelling of the joint cavity, which causes pain and joint stiffness when the joint capsule is stretched.
Continuous joints of bones are phylogenetically older. The lower animals have exclusively continuous connections. In humans, most of the bones are discontinuous connections. This is a later, most perfect and most mobile type of connection, although less durable. Discontinuous connections occur from continuous ones by their gradual transformation.
The bone underlying damaged articular cartilage also responds to the thickening by creating irregularities and causing the articular surface of the bone to become rough or bumpy. joint movement then leads to pain and inflammation. On early stages Osteoarthritis symptoms can be relieved by mild activity that "warms up" the joint, but symptoms may worsen after exercise. In those with more advanced osteoarthritis, the affected joints may become more painful and therefore difficult to use effectively, leading to increased immobility.
The emergence of a different nature of bone joints can also be observed in human ontogenesis. Similar to the stages of bone development, the development of their joints also occurs. In the early stages of the formation of the skeleton, the rudiments of the bones are connected to each other only by the embryonic connective tissue. Depending on the functional orientation, where there is no need for large-scale movements between the connecting bones, connective tissue remains, which can turn into cartilage to provide mobility and shock absorption, or into bone. This is how continuous connections are formed. Where greater mobility between the bones is needed, the connective tissue is resorbed, an interrupted connection occurs, with a cavity between the bones. The cavity appears by the end of the 2nd month of embryonic life.
There is no cure for osteoarthritis, but several treatments relieve pain. Treatment may include lifestyle changes such as weight loss and low-impact exercise, as well as over-the-counter or prescription medications to help relieve pain and inflammation. For severe cases, joint replacement surgery may be required.
Joint replacement is a very invasive procedure, so other treatments are always checked before surgery. However, arthroplasty can help relieve chronic pain and may improve mobility for several months after surgery. This type of surgery involves replacing the articular surfaces of bones with a prosthesis. For example, in hip arthroplasty, worn or damaged parts of the hip joint, including the head and neck of the femur and the acetabulum of the pelvis, are removed and replaced with artificial joint components.
All the bones in the human body, and there are more than two hundred of them, are interconnected. In anatomy, there is a section devoted to the doctrine of the joints of bones, which is called artrosyndesmology(from the Greek "arthron" - joint, "syndesmos" - ligament and "logos" - science). All bone joints are divided into three types (Fig. 1).
I. Continuous connections – synarthrosis, synarthroses. These are such connections when any tissue connecting them is located between the connecting bones. Basically, these are sedentary connections.
II. Intermittent connections – diarthrosis, diarthroses, or joints, articulation. These are such connections when there is a slit-like articular cavity between the connecting bones. For the most part, these are fairly mobile connections.
The femoral replacement socket consists of a rounded ball attached to the end of a shaft that is inserted inside the shaft of the femur. The acetabulum of the pelvis has been reshaped and a replacement socket inserted. Parts, which are always created prior to surgery, are sometimes custom made to ensure the best fit for the patient.
Gout is a form of arthritis that results from the deposition of uric acid crystals inside a joint. Usually only one or a few joints are affected, such as the thumb, knee, or ankle. The attack may only last a few days, but may return to the same or a different joint. Gout occurs when the body makes too much uric acid or the kidneys don't excrete it properly. A diet high in fructose has been associated with an increased chance of a susceptible individual developing gout.
III. Half joints, or symphyses, symphysis. These are such connections when a layer of connective or cartilaginous tissue is located between the connecting bones, in which there is a small gap.
CONTINUOUS BONE JOINTS
Depending on the type of tissue located between the bones and connecting them, all synarthroses are divided into four types:
Other forms of arthritis are associated with various autoimmune diseases, bacterial joint infections, or unknown genetic causes. Autoimmune diseases, including rheumatoid arthritis, scleroderma, or systemic lupus erythematosus, cause arthritis because the body's immune system attacks the body's joints. At rheumatoid arthritis the joint capsule and synovial membrane become inflamed. As the disease progresses, the articular cartilage is severely damaged or destroyed, leading to joint deformity, loss of motion, and severe disability.
1. Syndesmoses, syndesmoses - connections through connective tissue;
2. Synchondrosis, synchondroses - connections through cartilage tissue;
3. Synostoses, synostoses - connections through bone tissue;
4. Synsarcoses, synsarcoses - connections through muscle tissue.
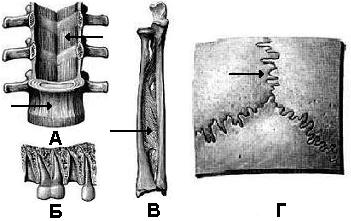
1. Syndesmoses can be represented by ligaments, interosseous membranes, impaction, sutures (Fig. 2).
The most common joints are the arms, legs, and cervical spine, with the corresponding joints on both sides of the body usually affected, though not always to the same extent. Rheumatoid arthritis is also associated with pulmonary fibrosis, vasculitis, ischemic disease heart disease and premature death. In the absence of a known cure, treatment is aimed at relieving symptoms. Treatments for rheumatoid arthritis include exercise, anti-inflammatory and pain medications, various specific disease-modifying antirheumatic drugs, or surgery.
Bundles, ligamenta are relatively thick bundles of dense fibrous or elastic connective tissue. For the most part, ligaments are thrown across the joint from one bone to another.
Interosseous membranes, membranae interosseae - these are flat connective tissue (formations) plates located between the bones. For example, interosseous membranes between the diaphyses of the bones of the forearm and lower leg.
Osteoarthritis of the synovial joint is caused by aging or prolonged wear and tear of the joints. This causes erosion and loss of the articular cartilage that covers the surfaces of the bones, leading to inflammation that causes joint stiffness and pain. Visit this site to learn about a patient who arrived at the hospital with joint pain and leg weakness. What caused this patient's weakness?
Watch this animation to watch hip replacement surgery, which can be used to relieve pain and loss of joint mobility associated with hip osteoarthritis. What is the most common cause of hip disability?
 Injections, gomphosis - are represented by a thin layer of connective tissue between the connecting structures. This is how the roots of the teeth are connected to the bone tissue of the dental alveoli. This layer of tissue is called periodontal, periodontum.
Injections, gomphosis - are represented by a thin layer of connective tissue between the connecting structures. This is how the roots of the teeth are connected to the bone tissue of the dental alveoli. This layer of tissue is called periodontal, periodontum.
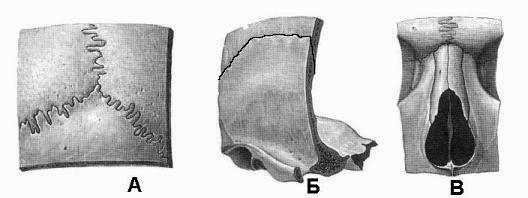
 seams, sutura - very thin layers of connective tissue located between the edges of the bones, for example, between the edges of the bones of the skull. Depending on the shape of the edges of the connecting bones, three types of sutures are distinguished:
seams, sutura - very thin layers of connective tissue located between the edges of the bones, for example, between the edges of the bones of the skull. Depending on the shape of the edges of the connecting bones, three types of sutures are distinguished:
Watch this video to learn about the symptoms and treatment of rheumatoid arthritis. What body system is disrupted in rheumatoid arthritis and what does this mean? Synovial joints are the most common type of joint in the body. They are characterized by the presence of an articular cavity, inside which the bones of the joint interlock with each other. The articulating surfaces of the bones at a synovial joint are not directly connected to each other by connective tissue or cartilage, allowing the bones to move freely against each other.
A) notched seam, sutura serrata, when the teeth of the edge of one bone go between the teeth of the edge of another, for example, the seam between the edges of the parietal bones;
b) scaly seam, sutura squamosa, when the oblique edges of the bones overlap each other, for example, the suture between the parietal and temporal bones;
V) flat seam, sutura plana, when the edges of the connecting bones are smooth, for example, the seams between the bones of the facial skull.
The walls of the joint cavity are formed by the articular capsule. Friction between bones is reduced by a thin layer of articular cartilage that covers the surfaces of bones and a lubricating synovial fluid that is secreted by the synovial membrane. Synovial joints are reinforced by the presence of ligaments that hold the bones together and resist excessive or abnormal movement of the joint. Ligaments are classified as external ligaments if they are located outside the joint capsule, internal ligaments if they are fused to the wall of the joint capsule, or intracapsular ligaments if they are located inside the joint capsule.
2. Synchondrosis may be represented by hyaline or fibrous cartilage. According to the duration of existence, synchondroses are temporary and permanent (Fig. 3).
Temporary synchondroses exist only at a certain age, and then are replaced by bone tissue - synostoses, for example, synchondrosis between the epiphysis and diaphysis tubular bones, between the sphenoid and occipital bones.
Some synovial joints also have an articular disc, which can provide padding between the bones, smooth their movements, or firmly hold the bones together to strengthen the joint. The muscles and their tendons acting through the joint can also increase their contractile force when needed, providing indirect support to the joint.
The burs contain a lubricating fluid that serves to reduce friction between the structures. The subcutaneous bursae prevent friction between the skin and underlying bone, the axillary bursae protect muscles from rubbing against bone or other muscle, and the subcutaneous bursa prevent friction between bone and muscle tendon. The tendon sheaths contain the lubricating fluid and tendons of the bulk joint to ensure smooth movement of the tendon as it crosses the joint.
Permanent synchondrosis exist throughout a person's life, for example, between the pyramid temporal bone And sphenoid bone, between the pyramid of the temporal bone and the occipital bone.
4. Synsarcoses- these are such joints of bones when muscle tissue is located between the connecting bones, for example, the joints of the scapula with the ribs and vertebrae, the hyoid bone with the lower jaw, sternum and scapula (Fig. 4).
Based on the shape of the articular surfaces of the bone and the types of movement allowed, synovial joints are classified into six types. At a hinge joint, one bone is held within the annulus by a ligament and its articulation with a second bone. Swivel joints allow only rotation around one axis. They are found at the articulation between C1 and the teeth of the C2 vertebrae, which provides transverse rotation of the head, or at the proximal radial joint between the head of the radius and the radial notch ulna, which allows the radius to rotate as the forearm moves.
All types of continuous connections, with the exception of synostoses, have one or another degree of mobility, which depends on the thickness of the layer of tissue connecting them. The larger the layer of connective, cartilaginous or muscle tissue, the more mobile these types of synarthroses. Phylogenetically continuous compounds are more ancient with a limited range of motion.
Articulations, for example, in the elbow, knee, ankle or interphalangeal joints between the bones of the phalanx of the fingers and toes, only allow bending and straightening of the joint. Hinges and articulated joints are functionally classified as uniaxial joints.
Condyloid joints occur where a shallow depression of one bone is given a rounded bony area formed by one or two bones. Condyloid joints occur at the base of the fingers and at the wrist. At the saddle joint, the articulating bones fit together like a rider and a saddle. An example is the first carpometacarpal joint located at the base thumb. Both condyloid and saddle joints are functionally classified as biaxial joints.
Below is a diagram of the types of continuous connections of bones.
Scheme 1
BASIC ELEMENTS OF THE JOINT
The main elements of the joint (Fig. 5) include the following formations:
1. 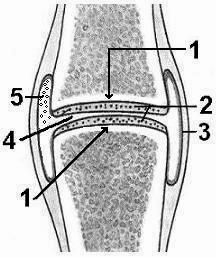 Articular surfaces, facies articulares;
Articular surfaces, facies articulares;
Flat sutures are formed between the small, flattened surfaces of adjacent bones. These joints allow bones to slide or rotate against each other, but the range of motion is usually negligible and tightly limited by ligaments or surrounding bones. This type of joint is found between the articular processes of neighboring vertebrae, in the acromioclavicular joint or in the intercarpal joints of the hand and interspherical joints of the foot. in the shoulder and hip joints there are articulated joints in which the rounded head of the bone is inserted into a large recess or socket.
2. articular cartilage, cartilago articulationes;
3. joint capsule, capsula articularis;
4. Articular cavity, cavitas articularis;
5. synovial fluid Liquor synovialis,
 1. Articular surfaces of bones are those parts that are adjacent to each other. If the articular surfaces of articulating bones along its area and shape correspond to each other, then they are spoken of as congruent surfaces (from the Latin “congruens” - proportionate, corresponding, coinciding). If the articular surfaces do not match in area and shape, they are said to be incongruent.
1. Articular surfaces of bones are those parts that are adjacent to each other. If the articular surfaces of articulating bones along its area and shape correspond to each other, then they are spoken of as congruent surfaces (from the Latin “congruens” - proportionate, corresponding, coinciding). If the articular surfaces do not match in area and shape, they are said to be incongruent.
2. articular cartilage covers articular surfaces, giving them a perfectly smooth surface. It is resilient and elastic. Usually it is hyaline cartilage, 0.2 - 5 mm thick. The layer of cartilage adjacent to the articular surface of the bone is calcified, which prevents the cartilage from being embedded into bone tissue even under high mechanical loads.
There are no vessels in the cartilage, and its nutrition is based on diffusion and osmosis of nutrients from the joint fluid.
Function articular cartilage is to increase the congruence of the articular surfaces, provide cushioning, reduce friction.
3. joint capsule(bag) is attached to the edges of the articular surfaces of the bones. Its thickness in the joints and even in one joint is different. The degree of tension of the capsule also varies. The articular bag of any joint consists of two layers.
A) Fibrous outer layer, membrana fibrosa (stratum fibrosum). It is formed from bundles of collagen and elastic fibers that are woven into the periosteum along the edges of the articular surfaces of the bones.
b) Synovial inner layer, membrana synovialis (stratum synoviale). This layer consists of loose connective tissue, contains many receptors, blood and lymphatic vessels. The synovial membrane is closely connected with the fibrous membrane and passes to the surfaces of the bones facing the joint cavity, but not covered by articular cartilage. If there are ligaments in the joint cavity or a tendon passes through it, then they are also covered with a synovial membrane.
On the inner surface of the synovial membrane, especially at the attachment of the articular bag to the bone, there are microscopic synovial villi, villi synoviales. Their number is directly proportional to the functional load of the joint and the age of the person.
Function of the articular capsule consists in the consolidation (strengthening) of the articular articular surfaces, providing biological and mechanical protection of the joint, performing receptor function(pain, baro- and mechanoreception), participation in metabolic processes(trophic) joint.
4. Articular cavity represents a hermetically closed slit-like space, limited directly by the articular cartilage and the synovial membrane of the bag. The pressure in the joint cavity is negative.
Function of the articular cavity is to retain the intra-articular fluid, the maximum convergence due to the negative pressure of the articular surfaces of the bones.
5. synovial fluid. It is located in the articular cavity in a volume of 0.1-4.0 ml. Normally transparent, viscous, with a specific gravity of 1010. It contains 95% water and up to 3% protein.
Function synovial fluid is to increase the adhesion forces between the articular surfaces of the bones, to nourish the articular cartilage, to reduce the friction forces between them, to maximize the congruence between the articular surfaces, to increase depreciation.
The structure of the joint
Joint classification
I. According to the number of articular surfaces, they distinguish:
1. The joints are simple, artt. simplexa,
2. The joints are complex, artt. composite,
3. Complex joints, artt. complexa.
4. Combined joints, artt. combinare,
(the concept is functional).
II. According to the shape of the articular surfaces are distinguished:
1. Cylindrical joint, art. trochoidea, this is the main form; its varieties:
a) block joint, art. ginglymus,
b) helical joint, art. cochlearis,
2. Elliptical joint, art. ellipsoidea, this is the main form; its varieties:
a) saddle joint, art. sellaris,
b) condylar joint, art. condylaris,
3. Ball joint, art. spheroidea, this is the main form; its varieties:
a) cup-shaped joint, art. cotylica,
b) flat joint, art. plana.
III. According to the number of axes of movement, they distinguish:
Uniaxial joints
Biaxial joints
Multiaxial joints
BIOMECHANICS OF JOINTS
In each joint, certain types of movements occur, the amplitude of which depends on the structure of the joint and its functional purpose. There are four main types of movements:
1. Movement around the frontal axis:
a) bending, flexio;
b) extension, extensio.
2. Movement around the sagittal axis:
a) reduction, adductio;
b) abduction, abductio.
3. Movement around a vertical axis
rotation(rotation):
a) internal rotation, pronatio;
b) outward rotation, supinatio.
4. Roundabout Circulation, circumductio, when a transition is made from one axis to another, and the proximal end of the bone rotates at the same point, and the distal end describes a circle. The whole bone as a whole outlines the figure of a cone.
Symphyses include transitional connections from continuous to discontinuous. These joints do not have an articular capsule, and in the cartilage located between the connecting bones there is a slit-like cavity with a small amount of fluid, but it is not lined with a synovial membrane, for example, the intervertebral and pubic symphyses (Fig. 7). In the symphyses, slight displacements of the connecting bones are possible.
Joints of the bones of the skull
Almost all the bones of the skull are interconnected by continuous joints. Only two bones - the temporal and lower jaw are connected through a joint - the temporomandibular.
The bones of the base of the skull are connected by synchondroses , for example, stony-occipital synchondrosis, synchondrosis petrooccipitalis. This synchondrosis connects the pyramid of the temporal bone with the basilar part of the occipital bone.
The bones of the cranial vault are connected by syndesmoses , represented by all three existing types of seams (Fig. 2 and 8).
 |
1. Serrated sutures (they predominate in the skull). The largest of them:
a) sagittal suture, sutura sagittalis, connects the sagittal edges of the parietal bones;
b) coronal suture, sutura coronalis, connects the anterior edges of the parietal bones with the frontal;
c) lambdoid suture, sutura lambdoidea, connects the posterior edges of the parietal bones with the occipital.
2. Scaly sutures connect the scales of the temporal bone with the parietal and with the greater wing sphenoid bone.
3. Flat sutures are present between the bones of the facial skull.
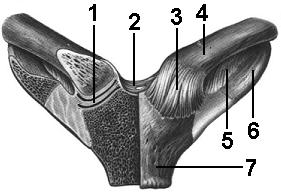
Temporomandibular joint, articulatio temporomandibularis . It has two articular surfaces (Fig. 9), presented head mandible , caput mandibulae, and mandibular fossa, fossa mandibularis, temporal bone. A feature of the joint is the presence in its cavity articular disc, discus articularis, which fuses around the circumference with the joint capsule and divides its cavity into the upper and lower floors. The disk provides an increase in the congruence of the articular surfaces and the range of motion in the joint.
![]() The joint has three ligaments:
The joint has three ligaments:
1. Lateral ligament , ligamentum laterale. It starts from the base zygomatic process temporal bone and ends on the posterolateral surface of the neck of the condylar process of the mandible. The ligament inhibits the movement of the head of the lower jaw backwards.
2.Sphenomandibular ligament, lig. sphenomandibular. It starts from the spine of the sphenoid bone and ends on the tongue of the lower jaw.
 3.Stylomandibular ligament, lig. stylomandibulare. It starts from styloid process and ends on the inner surface of the posterior edge of the lower jaw branch. Both ligaments provide stable fixation of the lower jaw.
3.Stylomandibular ligament, lig. stylomandibulare. It starts from styloid process and ends on the inner surface of the posterior edge of the lower jaw branch. Both ligaments provide stable fixation of the lower jaw.
Morphofunctional characteristics of the joint. The joint is simple, complex, combined, elliptical. The presence of an intra-articular disc in the joint cavity makes it possible to perform three types of movements in them when chewing and talking:
1. Around the frontal axis, lowering and raising the lower jaw occurs, providing opening and closing of the mouth;
2. Pushing the lower jaw forward and returning to its original position (sliding movements);
3. Movement of the jaw to the right and left. With these movements, in one joint, the head of the lower jaw rotates around the vertical axis from the side to which the jaw moves, and in the opposite joint, a sliding displacement occurs.
lowering lower jaw - mm. digastrici, mm. geniohyoidei, mm. mylohyoidei, mm. infrahyoidei
uplift lower jaw - mm. temporales, mm. masseter, mm. pterygoidei mediales
Advancement of the lower jaw- mm. pterygoidei laterales
Movement of the lower jaw back- mm. temporales (posterior bundles)
Movement of the lower jaw to the side- mm. pterygoideus lateralis (opposite side)
Joints of the bones of the body
I. VERTEBRAL JOINTS. They are interconnected by bodies, arcs and processes.
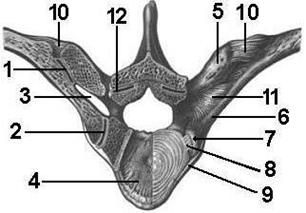
Vertebral bodies connected through intervertebral discs , disci intervertebrales, from 3-4 to 10-12 mm thick (Fig. 10).
The peripheral part of the disk is represented by fibrous cartilage, the fibers of which form annulus fibrosus anulus fibrosus. This type of connection refers to synchondrosis.
The central part of the disk is represented gelatinous nucleus, nucleus pulposus. Often there is a small gap in the nucleus, which allows this connection to be attributed to symphyses, namely to intervertebral symphyses, symphysis intervertebrales.
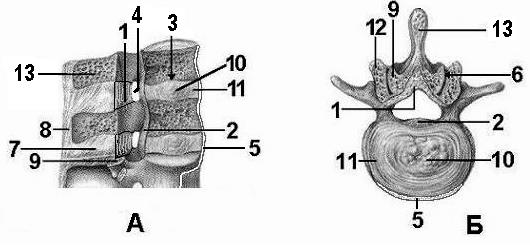 |
In addition to the intervertebral discs, the vertebral bodies are also connected using two ligaments:
A) anterior longitudinal ligament, lig. longitudinale anterius, which goes from the pharyngeal tubercle of the occipital bone and the anterior tubercle of the anterior arch of the atlas along the entire spinal column up to 2-3 transverse lines of the sacrum, firmly connected with the intervertebral discs;
b) posterior longitudinal ligament, lig. longitudinale posterius, which starts from the posterior surface of the body of the second cervical vertebra, passes inside spinal canal along the back surface of the vertebral bodies, attaching to them and to the intervertebral discs, and ends on the bodies of the sacral vertebrae.
2. Arcs of the vertebrae interconnected through yellow ligaments, ligg. flava (Fig. 11). These ligaments are very strong, elastic, have a yellowish color, fill the gaps between the arcs.
3. Processes of the vertebrae the transverse and spinous are connected by ligaments, and the articular processes are connected by joints.
The transverse processes connect intertransverse ligaments, ligg. intertransversaria (Fig. 11), connecting the tops of the processes of adjacent vertebrae. These links are missing from cervical region spinal column.
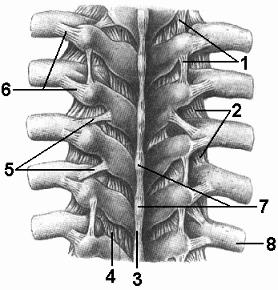 The spinous processes are connected to each other by two ligaments: a) interspinous– ligg. interspinalia, located between the spinous processes, and b) supraspinous– lig. supraspinale (Fig. 10, 11). This ligament is attached to the tops of all spinous processes. Part of this ligament in the cervical spine is a triangular-shaped plate located in the sagittal plane called nuchal ligament, lig. nuchae. At the top, this ligament is attached to the external crest of the occipital bone, in front - to the spinous processes of the cervical vertebrae, below - ends on the spinous process of the VII cervical vertebra and passes into the supraspinous ligament.
The spinous processes are connected to each other by two ligaments: a) interspinous– ligg. interspinalia, located between the spinous processes, and b) supraspinous– lig. supraspinale (Fig. 10, 11). This ligament is attached to the tops of all spinous processes. Part of this ligament in the cervical spine is a triangular-shaped plate located in the sagittal plane called nuchal ligament, lig. nuchae. At the top, this ligament is attached to the external crest of the occipital bone, in front - to the spinous processes of the cervical vertebrae, below - ends on the spinous process of the VII cervical vertebra and passes into the supraspinous ligament.
The articular processes of adjacent vertebrae are connected by facet or intervertebral joints , articulationes zygapophysiales seu intervertebrales (Fig. 12).
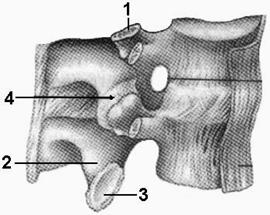
These joints are simple, combined, flat, multiaxial. Each of these joints is functionally inactive, but their combination provides large amplitude movements of the spinal column.
 Joints between the inferior articular processes of the last fifth lumbar vertebra and the upper articular processes of the sacrum are called lumbosacral joints, articulationes lumbosacrales. Their morphofunctional characteristics are the same as those of the intervertebral joints described above.
Joints between the inferior articular processes of the last fifth lumbar vertebra and the upper articular processes of the sacrum are called lumbosacral joints, articulationes lumbosacrales. Their morphofunctional characteristics are the same as those of the intervertebral joints described above.
Muscles that provide movement in the joint:
bending spinal column - mm. recti abdominis, mm. obliqui abdominis (externi et interni), mm.scaleni, mm. longi colli, mm. sternocleidomastoidei
Extension spinal column - m. erector spinae, m. transversospinalis, m. trapezius, mm. splenii capitis and cervicis
Lateral tilt of the spine- simultaneous action of flexors and extensors, mm. quadratus lumborum (corresponding side)
Twisting spinal column - m. transversospinalis, m. obliquus externus abdominis, mm.scaleni (of the corresponding side), m. obliquus internus abdominis et mm. splenii capitis et cervicis (opposite side)
4. sacrum with coccyx connected through sacrococcygeal joint , articulatio sacrococcygea . The joint is strengthened by four ligaments:
A) lateral sacrococcygeal ligament, lig. sacrococcygeum laterale;
b) ventral sacrococcygeal ligament, lig. sacrococcygeum ventrale;
V) superficial posterior sacrococcygeal ligament, lig. sacrococcygeum posterius superficiale;
G) deep posterior sacrococcygeal ligament, lig. sacrococcygeum posterius profundum.
The sacrococcygeal joint is of great importance in pregnant women. During childbirth, it allows the coccyx to deviate backwards and increase the outlet of the birth canal.
II. CONNECTIONS OF THE SPINE COLUMN TO THE SKULL. These connections are made between two bones: the occipital (from the side of the skull) and the atlas (from the side of the spine). These bones form two atlantooccipital joint , articulatio atlantooccipitalis , in which the articular fossae of the atlas are connected to the articular surfaces of the condyles of the occipital bone. Joints are strengthened anterior and posterior atlantooccipital membranes, membrana atlantooccipitalis anterior et posterior. These membranes are fixed: anterior - to the basilar part of the occipital bone and to the upper edge of the anterior arch of the atlas; posterior - to the semicircle of the foramen magnum and to the upper edge of the posterior arch of the atlas.
The joints are simple, combined, condylar, biaxial. Flexion and extension occur around the frontal axis, i.e. tilting the head forward and backward (nodding movements). Abduction and adduction of the head are performed around the sagittal axis, i.e. tilting the head to the right and left and returning it to its original position.
In addition to the atlantooccipital joints, three joints between the first two also take part in head movements. cervical vertebrae- atlas and axial vertebrae. These joints are called atlantoaxial.
Median atlantoaxial joint, articulatio atlantoaxialis mediana . This unpaired joint (Fig. 14) is formed by the anterior and posterior articular surfaces of the tooth of the axial vertebra, the fossa of the atlas tooth and its articular surface transverse ligament, lig. transversum atlantis. The ligament passes behind the tooth, fixing to the inner surfaces of the lateral masses of the atlas.
Morphofunctional characteristics of the joint. The joint is simple, cylindrical, uniaxial, combined. Movements (rotations) are performed only around the vertical axis. In this case, the atlas, together with the skull, rotates around the tooth.
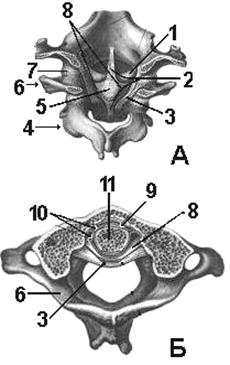 Two other pairs lateral joint between atlas and axial vertebra
, articulatio atlantoaxialis lateralis
(Fig. 14a), formed by the lower articular fossa on the lateral mass of the atlas and the upper articular surface on the body of the axial vertebra.
Two other pairs lateral joint between atlas and axial vertebra
, articulatio atlantoaxialis lateralis
(Fig. 14a), formed by the lower articular fossa on the lateral mass of the atlas and the upper articular surface on the body of the axial vertebra.
Morphofunctional characteristics of the joint. These joints are simple, combined, flat, multiaxial. During rotation in the median atlantoaxial joint, sliding movements occur in the lateral atlantoaxial joints.
All three atlanto-axial joints are reinforced with several ligaments.
 Ligament of the apex of the tooth, lig. apicis dentis, stretched between the anterior circumference of the foramen magnum and the apex of the tooth. Two pterygoid ligaments, ligg. alaria, are fixed to the lateral surfaces of the tooth and to the inner surfaces of the condyles of the occipital bone.
Ligament of the apex of the tooth, lig. apicis dentis, stretched between the anterior circumference of the foramen magnum and the apex of the tooth. Two pterygoid ligaments, ligg. alaria, are fixed to the lateral surfaces of the tooth and to the inner surfaces of the condyles of the occipital bone.
Behind these three ligaments is cruciate ligament of atlas, lig. cruciforme atlantis. It is formed by the transverse ligament of the atlas and fibrous longitudinal bundles, fasciculi longitudinales. These fibers are attached to the anterior semicircle of the foramen magnum and the posterior surface of the body of the axial vertebra.
Posteriorly, all three atlantoaxial joints with their ligaments are covered integumentary membrane, membrana tectoria. At the top, it is fixed on the inner surface of the basilar part of the occipital bone, and below it passes into the posterior longitudinal ligament of the spinal column.
bending heads - mm. recti capitis anteriores, mm. recti capitis laterales, mm. longi capitis, and with a fixed lower jaw - m. digastricus, m. stylohioides, m. mylohyoideus, m. geniohyoideus, m. omohyoideus, m. sternohyoideus, m. thyrohyoideus, m. sternothyroideus
Extension heads - mm. trapezii, mm. splenii capitis, mm. sternocleidomastoidei, mm. longissimi capitis, mm. semispinales capitis, mm. recti capitis posteriores majores et minores, mm. oblqui capitis superiores
Head tilt to the side- simultaneous action of flexors and extensors (of the respective side)
Turning the head to the side- mm. splenii capitis, mm. longissimi capitis, mm. oblqui capitis inferiores (of the respective party) and m. sternocleidomastoideus (opposite side)
III. JOINTS OF THE RIBS TO THE SPINE COLUMN. The ribs are connected to the vertebrae by costovertebral joints articulationes costovertebrales . Each of them consists of two joints: the joint of the head of the rib and the costotransverse joint.
 rib head joint,
articulatio capitis costae
(Fig. 15), formed by the articular surface of the head of the rib, the upper and lower fossae (half-fossae) of two adjacent thoracic vertebrae. At the II-X ribs from the crest of their heads to the intervertebral disc is located intraarticular ligament of head of rib, lig. capitis costae intraarticulare.
rib head joint,
articulatio capitis costae
(Fig. 15), formed by the articular surface of the head of the rib, the upper and lower fossae (half-fossae) of two adjacent thoracic vertebrae. At the II-X ribs from the crest of their heads to the intervertebral disc is located intraarticular ligament of head of rib, lig. capitis costae intraarticulare.
 The heads of the 1st, 11th, and 12th ribs do not have a comb and the aforementioned ligament. They are connected to the articular surfaces (pits) of the I, XI, XII vertebrae.
The heads of the 1st, 11th, and 12th ribs do not have a comb and the aforementioned ligament. They are connected to the articular surfaces (pits) of the I, XI, XII vertebrae.
The joint capsule is strengthened radiant ligament of head of rib, lig. capitis costae radiatum. The bundles of this ligament from the head of the rib are fan-shaped directed to the intervertebral disc and the bodies of the adjacent vertebrae.
Costotransverse jointarticulatio costotransversaria , formed by the articular surfaces of the tubercle of the rib and the costal fossa on the transverse process of the vertebra. The capsule is strengthened costotransverse ligament, lig. costotransversarium.
Morphofunctional characteristics of the joints. Both joints are simple, flat, combined, multiaxial, and provide raising and lowering of the anterior ends of the ribs.
IV. JOINING THE RIBS TO THE BREAST.
The cartilaginous parts of the 1st rib are connected to the sternum by means of synchondrosis. With the help of synchondroses, the cartilaginous parts of the VII, VIII, IX, X ribs are connected to each other.
The ends of the cartilaginous parts of the II-VII ribs are connected to the notches of the sternum through sternocostal joints , articulationes sternocostales (Fig. 16). Joint capsules are strengthened radiant sternocostal ligaments, ligg. sternocostalia radiata. In front, these ligaments fuse with the periosteum of the sternum, forming sternum membrane, membrana sterni.
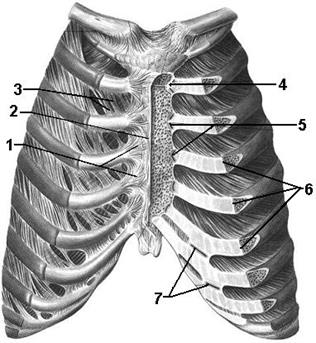 |
Morphofunctional characteristics of the joints. The joints are simple, combined, flat, multiaxial.
The anterior cartilaginous parts of the ribs are connected to each other in front of the anterior, and behind - by the posterior intercostal membranes, membrana intercostalis externa et interna.
Muscles that provide movement in the joints:
Raising the anterior ends of the ribs- mm. intercostales externi, mm. levatores costarum, mm. serrati posteriores superiores, mm. scaleni
Lowering the front ends of the ribs- m. transversus thoracis, mm. intercostales interni, mm. serrati posteriores inferiores, mm. recti abdominis, mm. obliqui abdominis (externi et interni), mm. transversi abdominis
UPPER LIMB JOINTS
I. JOINTS OF BONES OF THE BELT OF THE UPPER LIMB.
 The clavicle connects to the sternum and shoulder blade. It communicates with the sternum through sternoclavicular joint
, articulatio sternoclavicularis
(fig.17). The articular surfaces are the saddle surface of the sternal end of the clavicle and the clavicular notch of the manubrium of the sternum. Between these surfaces is the articular disc, discus articularis, dividing the articular cavity into two capsules.
The clavicle connects to the sternum and shoulder blade. It communicates with the sternum through sternoclavicular joint
, articulatio sternoclavicularis
(fig.17). The articular surfaces are the saddle surface of the sternal end of the clavicle and the clavicular notch of the manubrium of the sternum. Between these surfaces is the articular disc, discus articularis, dividing the articular cavity into two capsules.
 The joint capsule is strengthened by three ligaments: front And posterior sternoclavicular, ligg. sternoclavicularia anterius et posterius, and costoclavicular, lig. costoclaviculare. The costoclavicular ligament is very strong, connecting the lower surface of the sternal end of the clavicle with upper surface cartilage of the 1st rib.
The joint capsule is strengthened by three ligaments: front And posterior sternoclavicular, ligg. sternoclavicularia anterius et posterius, and costoclavicular, lig. costoclaviculare. The costoclavicular ligament is very strong, connecting the lower surface of the sternal end of the clavicle with upper surface cartilage of the 1st rib.
 The upper posterior surfaces of the sternal ends of both clavicles are connected by passing over the jugular notch interclavicular ligament, lig. interclaviculare.
The upper posterior surfaces of the sternal ends of both clavicles are connected by passing over the jugular notch interclavicular ligament, lig. interclaviculare.
 Morphofunctional characteristics of the joint. The joint is simple, complex, flat, triaxial (multiaxial). Around the sagittal axis, the clavicle rises and falls, and around the vertical axis, the clavicle moves forward and backward. Rotational movements of the clavicle around its longitudinal frontal axis are possible, but only when working together with the shoulder joint, during flexion and extension of the free joint in it. upper limb.
Morphofunctional characteristics of the joint. The joint is simple, complex, flat, triaxial (multiaxial). Around the sagittal axis, the clavicle rises and falls, and around the vertical axis, the clavicle moves forward and backward. Rotational movements of the clavicle around its longitudinal frontal axis are possible, but only when working together with the shoulder joint, during flexion and extension of the free joint in it. upper limb.
The clavicle is connected to the scapula by acromioclavicular joint , articulatio acromioclavicularis (fig.18). The articular surfaces are located at the acromial end of the clavicle and the inner edge of the acromion of the scapula. Between these surfaces in 1/3 of cases there is an articular disc, discus articularis.
The joint capsule is strengthened by two ligaments: from above - acromioclavicular, lig. acromioclaviculare, below - coracoclavicular, lig. coracoclaviculare. The last ligament is formed from two ligaments starting from the base of the coracoid process of the scapula and ending on the cone-shaped tubercle of the clavicle (lig. conoideum) and on its trapezoid line (lig. trapezoideum).
Morphofunctional characteristics of the joint. The joint is simple, complex in 1/3 cases, flat, low-amplitude movements occur around three axes.
Ligaments of the scapula. The scapula has three ligaments of its own, which have nothing to do with the described joints. Coracoacromial ligament, lig. coracoacromiale, stretched between the acromial and coracoid process of the scapula above the shoulder joint and prevents excessive abduction of the free upper limb in the shoulder joint.
Superior transverse ligament, lig. transversum scapulae superius, is located above the notch of the scapula, turning it into a hole.
Inferior transverse ligament of scapula, lig. transversum scapulae inferius, located between the base of the acromion and the posterior edge of the glenoid cavity of the scapula.
Muscles that provide movement in the joint:
Elevation of the collarbone and scapula- m. levator scapulae, mm. rhomboidei, m. sternocleidomastoideus, m. trapezius (upper bundles)
Descent of the collarbone and scapula- m. trapezius, m. serratus anterior (lower bundles), m. pectoralis minor, m. subclavius
Movement clavicle forward(shoulder blades - to the lateral side) - m. serratus anterior, m. pectoralis minor, m. pectoralis major. Movement clavicle back(shoulder blades - to the medial side) - m. trapezius, mm. rhomboidei, m. latissimus dorsi
Pronation shoulder blades (turning the lower angle outward) - m. serratus anterior (lower teeth), m. trapezius (upper bundles). Supination shoulder blades (rotation by the lower angle inwards) - mm. rhomboidei, m. pectoralis minor
II. FREE UPPER LIMB JOINTS
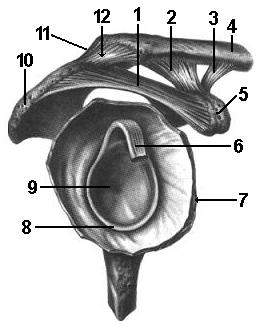
shoulder joint , art. humeri . It articulates the free upper limb with its belt (Fig. 19) by connecting the surface of the articular cavity of the scapula and head humerus. The congruence of the glenoid cavity of the scapula is increased by articular lip, labrum glenoidale, which is attached along the edges of the cavity.
The joint capsule is thin, free, allowing the articular surfaces to move away from each other up to 2-3 cm. There is only one coracohumeral ligament, lig. coracohumerale. It's thickened top part joint capsule, up to 3 cm wide, located between the base of the coracoid process of the scapula and top anatomical neck of the humerus.
The synovial membrane of the joint has two protrusions: the first of them is intertubercular synovial sheath, vagina synovialis intertubercularis, envelops the tendon of the long head of the biceps brachii; the second is dry bag subscapularis muscle, bursa subtendinea m. subscapularis, at the base of the coracoid process.
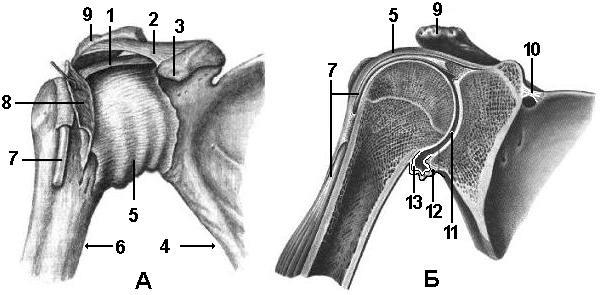 |
Morphofunctional characteristics of the joint. The shoulder joint is simple, spherical, triaxial (multiaxial). The structure of the joint determines its greatest mobility in the human body. Flexion and extension of the upper limb occurs around the frontal axis, abduction and adduction around the sagittal axis, supination and pronation around the vertical axis. In the joint, it is also possible circular motions(circumduction).
When the limb moves above the level of the shoulder, all joints of the girdle of the upper limb are included in the work.
Muscles that provide movement in the joint:
bending shoulder - m. deltoideus (front bundles), m. pectoralis major, m. biceps brachii, m. coracobrachialis.
Extension shoulder - m. deltoideus (posterior bundles), m. triceps brachii (long head), m. latissimus dorsi, m. teres major, m. infraspinatus.
lead shoulder - m. deltoideus, m. supraspinatus.
Casting shoulder - m. pectoralis major, m. latissimus dorsi, m. subscapularis, m. infraspinatus.
Pronation shoulder - m. deltoideus (front bundles), m. pectoralis major, m. latissimus dorsi, m. teres major, m. subscapularis.
Supination shoulder - m. deltoideus (posterior bundles), m. teres minor, m. infraspinatus
elbow joint , articulatio cubiti . In this joint, the articular surfaces of three bones are articulated: the humerus, ulna and radius (Fig. 20). Articulating bones form three joints enclosed in one capsule:
1. Shoulder joint, articulatio humeroulnaris, is formed by a block of the humerus and a block-shaped notch of the ulna. The joint is simple, helical (a kind of blocky), uniaxial.
2. Shoulder joint, articulatio humeroradialis, formed by the head of the humerus and the articular fossa of the head radius. The joint is simple, spherical, triaxial.
3. Proximal radioulnar joint, articulatio radioulnaris proximalis, is formed by the circumference of the radius and the radial notch of the ulna. The joint is simple, cylindrical, uniaxial.
The capsule of the elbow joint is relatively free. In the joint cavity are the coronal and ulnar fossa of the humerus, as well as the olecranon of the ulna. The joint has three ligaments. Located on the sides ulnar And radial collateral ligament, ligg. collaterale ulnare et radiale. The ulnar collateral ligament connects the medial epicondyle of the humerus to the edge of the trochlear notch of the ulna. The radial collateral ligament starts from the lateral epicondyle, covers the neck of the radius with two legs in front and behind, and ends at the anterolateral edge of the trochlear notch of the ulna and in the annular ligament.
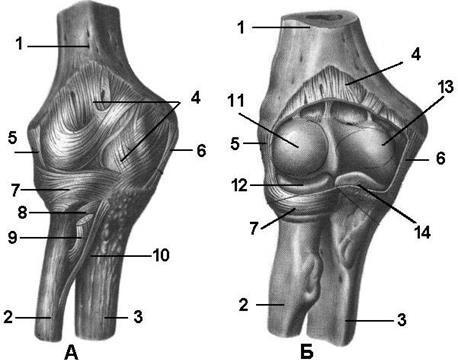 Third annular ligament radius, lig. annulare radii, is represented by fibrous fibers that arc around the neck and head of the radius and are fixed to the edges of the radial notch of the ulna.
Third annular ligament radius, lig. annulare radii, is represented by fibrous fibers that arc around the neck and head of the radius and are fixed to the edges of the radial notch of the ulna.
Morphofunctional characteristics of the joint. The elbow joint is a complex joint, and movements in it are possible in two ways. Around the frontal axis, flexion and extension of the forearm occurs, and movements are carried out in the humeroulnar and humeroradial joints.
Around the vertical axis, rotation (supination and pronation) occurs in the proximal and distal humeroradial joints, because these joints are combined.
Muscles that provide movement in the joint:
bending forearms - m. brachialis, m. biceps brachii, m. pronator teres
