The nasal cavity includes the vestibule and the nasal (respiratory) cavity proper. The vestibule is lined with thin skin containing sebaceous, sweat glands and hair follicles. The respiratory cavity is lined with a mucous membrane that has replaced thin skin; here the epidermis passes into a multi-row ciliated epithelium containing goblet, basal cells and cells with microvilli. The own layer of the mucous membrane contains collagen and elastic fibers, as well as mucous and protein glands that produce a large number of mucus.
Larynx
The larynx is the upper part of the airways; the main function, in addition to conducting air, is voice formation. It is separated from the pharynx by the epiglottis, and in the lower part it is limited by the first cartilaginous semicircle of the trachea. It has mucous, fibrocartilaginous and adventitial membranes. The composition of the fibrocartilaginous membrane of the larynx includes 4 cartilages - epiglottic, thyroid, arytenoid, cricoid. The epithelium of the mucous membrane (with the exception of the vocal cords) is multi-row ciliated. The own layer of the anterior surface of the larynx contains mixed protein-mucous glands, accumulations of lymphatic follicles.
Vocal cords - the upper and lower folds of the mucous membrane in the middle part of the organ, forming, respectively, false and true vocal cords. The space between the true vocal cords is the glottis. The area of expansion of the lumen of the larynx between the two rows of ligaments is the ventricle of the larynx. The basis of the false vocal cords is loose connective tissue containing protein-mucous glands. Such glands are also present above and below the true vocal cords. The true vocal cords contain bundles of striated muscle fibers; glands are absent. Both types of vocal cords, like the anterior surface of the epiglottis, are covered with stratified squamous nonkeratinized epithelium.
Trachea
The wall of the trachea is formed by the mucous, submucosal, fibrocartilaginous and adventitious membranes.
Mucous shell
The mucous membrane consists of a single layer of multi-row ciliated epithelium and a thin layer of its own. The muscle layer is missing. The proper mucosal layer contains numerous elastic fibers and few mucous glands. Individual lymphocytes and lymphatic follicles are found here.
Epithelium The trachea contains various types of cells. Ciliated cells make up the bulk of the epithelium. Among the ciliated goblet, basal, brush (border), neuroendocrine, chemoreceptor cells are scattered.
Trachea. The wall is formed by four shells. The mucous membrane (1) consists of a multi-row ciliated epithelium and its own layer. The submucosa (2) is characterized by numerous mucous and protein-mucous glands. The fibrocartilaginous membrane (3) is represented by open rings of hyaline cartilage. The adventitia (4) is formed by fibrous connective tissue. Stained with hematoxylin and eosin.
Stratified epithelium of the tracheal mucosa. The epithelium consists of various types of cells. The first (main) type ( 1 ) - ciliated cells with more than 200 cilia on the apical surface. The second type ( 2 ) - high goblet cells containing vacuoles with a mucous secretion in the apical part, and in the basal part - the nucleus and various organelles. The third type ( 3 ) - basal (stem) cells that are small in size. fourth type ( 4 ) - brush (border) cells. Fifth type ( 5 ) - chemoreceptor cells containing fine granularity and forming contact with afferent terminals. sixth type ( 6 ) - neuroendocrine cells with numerous small granules.
Submucosal shell
The boundary between the mucosa and submucosa is a compacted plate of intertwined elastic fibers. The submucosa contains many blood vessels and secretory sections of the mucous and protein-mucous glands.
Fibrocartilaginous shell
The fibrocartilaginous membrane is represented by plates in the form of open rings of hyaline cartilage, surrounded by a thin fibrous membrane - the perichondrium. The ends of the rings are connected by bundles of connective tissue fibers and MMC. Neighboring rings are interconnected by a dense connective tissue (intertwined collagen and individual elastic fibers), passing into the perichondrium of the rings.
The adventitia is made up of fibrous connective tissue.
The wall of the trachea.
Bronchi
The structure of the bronchi is similar to the structure of the trachea, but there are certain differences.
mucous membrane
The mucous membrane of the bronchi, unlike the trachea, has a muscular layer. This layer consists of MMCs arranged in the form of two oppositely directed (clockwise and counterclockwise) spirals. The contraction of the SMC leads to the formation of longitudinal folds of the bronchial mucosa. The intrinsic mucosal layer contains many elastic fibers arranged in several long ribbons running in parallel. The ribbons pass into the elastic components of the terminal bronchioles. The epithelium of the bronchial mucosa is a single-layer multi-row cylindrical ciliated, it contains ciliated, goblet, border, endocrine and basal cells.
Submucosal shell
The submucosa contains mucous and protein-mucous glands. The glands are located in groups, especially in those areas where there is no cartilage. There are no glands in the bronchi of small caliber.
Fibrocartilaginous shell
Cartilage in the form of open rings, present in the main bronchi, in large intrapulmonary bronchi are replaced by irregularly shaped cartilaginous plates, and then islets of cartilaginous tissue (medium-sized bronchi). The spaces between the cartilages are filled with connective tissue passing into the perichondrium. There is no cartilaginous tissue in the bronchi of small caliber.
The airways, which include the fibrocartilaginous membrane, do not collapse, their lumen has an almost constant diameter, but the diameter of the terminal sections of the bronchial tree changes, which is possible due to the relative development of the muscularis mucosa and the absence of a cartilaginous framework. The change in the size of the lumen of the bronchi is also affected by the folds of the mucous membrane, the degree of development of elastic fibers in it. Pay attention to the mechanisms of regulation of the tone of smooth myocytes (neurotransmitters and hormones).
outdoor shell.
The adventitial membrane is a connective tissue that passes into the interlobar and interlobular connective tissue of the lung parenchyma.
Bronchus of medium caliber. The mucous membrane is lined with multi-row cylindrical ciliated epithelium (1), has a muscular layer (2). Mucous glands are present in the submucosa (3). The fibrocartilaginous membrane contains plates of hyaline cartilage (4). Alveoli are visible around the bronchus (5), blood vessels pass through the connective tissue septa of the lung parenchyma (6). Stained with hematoxylin and eosin.
Bronchioles
Bronchioles differ from bronchi in a number of ways: their diameter is much smaller and ranges from 0.5 to 1 mm. The epithelium of the mucous membrane is single-row cylindrical ciliated; its height is less than in the bronchi. In the epithelium of larger bronchioles, ciliated cells predominate, between which bronchiolar exocrinocytes are located. Cartilage and glands are absent in the wall of bronchioles. Thus, the wall of bronchioles consists of the following elements: a single-row cylindrical (cubic) epithelium, a thin and elastic layer of its own, a muscular layer of the mucous membrane and external connective tissue. In total, 20 generations of bronchioles are formed, the smallest of which are terminal
Outside, the nose consists of wings, or nostrils, a back - the middle part and a root located in the frontal lobe of the face. Inside its walls are formed by the bones of the skull, and from the side of the mouth it is limited to a hard and soft palate. It has a complex structure - the nasal cavity is divided into two nostrils, each of which has a medial (partition between the nostrils), lateral, upper, lower and rear walls.
In addition to bone tissue, the structure of the nasal cavity includes membranous and cartilaginous components, which are characterized by high mobility. There are three shells in the cavity- upper, middle and lower, but only the last true, since it alone is formed by an independent bone. Between the shells there are passages - spaces through which air flows pass:
top move. It is located behind and has holes in the cell of the ethmoid bone;
average move. It communicates with its anterior cells, with the frontal and maxillary sinuses;
bottom move. It connects through the nasolacrimal duct to the orbit.
The nasal cavity consists of the vestibule and the respiratory part.
The vestibule of the nose is lined with a mucous membrane, which includes a stratified squamous non-keratinized epithelium and a lamina propria.
The respiratory part is lined with a single-layer multi-row ciliated epithelium. In its composition are distinguished:
ciliated cells - have ciliated cilia, oscillating against the movement of the inhaled air, with the help of these cilia, microorganisms and foreign bodies are removed from the nasal cavity;
goblet cells secrete mucins - mucus that sticks together foreign bodies, bacteria and facilitates their removal;
microvillous cells are chemoreceptor cells;
basal cells play the role of cambial elements.
The lamina propria is formed by loose fibrous unformed connective tissue, it contains simple tubular protein-mucous glands, vessels, nerves and nerve endings, as well as lymphoid follicles.
The mucous membrane lining the respiratory part of the nasal cavity has two areas that differ in structure from the rest of the mucous membrane:
the olfactory part, which is located on most of the roof of each nasal cavity, as well as in the superior turbinate and the upper third of the nasal septum. The mucous membrane lining the olfactory regions forms the organ of smell;
the mucous membrane in the region of the middle and inferior turbinates differs from the rest of the nasal mucosa in that it contains thin-walled veins resembling the lacunae of the cavernous bodies of the penis. AT normal conditions the blood content in the lacunae is small, as they are in a partially collapsed state. When inflammation (rhinitis) occurs, the veins become congested with blood and narrow the nasal passages, making it difficult to breathe through the nose.
The olfactory organ is the peripheral part of the olfactory analyzer. The olfactory epithelium consists of three types of cells:
olfactory cells are spindle-shaped and have two processes. The peripheral process has a thickening (olfactory club) with antennae - olfactory cilia that run parallel to the surface of the epithelium and are in constant motion. In these processes, upon contact with odorous substance, a nerve impulse is formed, which is transmitted along the central process to other neurons and further to the cortex. Olfactory cells are the only type of neurons that have a precursor in the form of cambial cells in an adult individual. Thanks to the division and differentiation of the basal cells, the olfactory cells are renewed every month;
supporting cells are located in the form of a multi-row epithelial layer, on the apical surface they have numerous microvilli;
basal cells are conical and lie on the basement membrane at some distance from each other. Basal cells are poorly differentiated and serve as a source for the formation of new olfactory and supporting cells.
The lamina propria of the olfactory region contains the axons of the olfactory cells, the choroid venous plexus, and the secretory sections of the simple olfactory glands. These glands produce a protein secret and release it to the surface of the olfactory epithelium. The secret dissolves odorous substances.
The smell analyzer is built from 3 neurons.
The first neuron is the olfactory cells, their axons form the olfactory nerves and end in the form of glomeruli in the olfactory bulbs on the dendrites of the so-called mitral cells. This is the second link of the olfactory pathway. Axons of mitral cells form olfactory pathways in the brain. The third neurons are cells of the olfactory pathways, the processes of which end in the limbic region of the cerebral cortex.
The nasopharynx is a continuation of the respiratory part of the nasal cavity and has a structure similar to it: it is lined with multi-row ciliated epithelium lying on its own plate. The secretory sections of small protein-mucous glands lie in the lamina propria, and on the posterior surface there is an accumulation of lymphoid tissue (pharyngeal tonsil).
The structure of the paranasal sinuses.
The paranasal sinuses consist of several parts that are interconnected.
The maxillary sinus is an air cavity adjacent to the nasal cavity and communicating with it through the maxillary foramen, which opens into the middle nasal passage. The paranasal sinuses, which include the maxillary sinus, appear in the form of rudiments in the embryonic period of fetal development; changing shape and size, they continue to develop in the postnatal period and finally form at the age of 14-20 years.
Maxillary sinus- the largest paranasal sinus. It is located in the depth upper jaw and in shape resembles a triangular pyramid, the base of which is the outer wall of the nasal cavity, and the apex is the zygomatic process of the upper jaw. The capacity of the sinus ranges from 3-30 cm3, averaging 10-12 cm3. The air pressure in it is normally the same as in the nasal cavity.
The volatility of the volume of the sinus is explained by the conditions of its development.
It was found that the maxillary sinus is formed due to the resorption of the spongy substance of the upper jaw. It is possible that this process is influenced by the function of the masticatory apparatus. In cases where resorption occurs slowly and ends sooner, the dimensions of the maxillary sinus are so small that it can be taken as rudimentary; the walls of such a sinus are thick. Good bone resorption leads to the formation of a large sinus. According to German doctors, narrowing of the maxillary sinus can also occur as a result of: 1) convergence of the outer and inner walls of the sinus with each other; 2) strong protrusion of the nasal wall and towards the maxillary sinus; 3) thickening of the walls of the maxillary sinus; 4) retention of teeth in the alveolar process; 5) combinations of all these conditions.
The inner wall of the maxillary sinus is the outer wall of the nasal cavity. This wall is the most complex anatomically and is of great clinical importance. It consists of the nasal bones, the medial surface of the body of the upper jaw with the frontal process, the lacrimal bone, the cells of the ethmoid labyrinth, the perpendicular plate of the palatine bone and the inner plate of the pterygoid process of the sphenoid bone.
The inner wall of the maxillary sinus is mainly projected onto the lower and middle nasal passages. The bone wall gradually becomes thinner from bottom to top and from front to back and is completely absent in the central part of the middle nasal passage. Here the wall consists of a duplication of the mucosa.
On the inner wall of the maxillary sinus at the base of the orbit there is a hole through which the maxillary sinus communicates with the nasal cavity in the region of the anterior middle nasal passage.
The size of the hole is 2-19 mm long and 2-6 mm wide. The hole located on the wall of the sinus does not strictly correspond to the mouth of the sinus in the nasal cavity and can be distant from it at a distance of 1 cm, resulting in the formation of an oblique canal. This circumstance, combined with the high position of the opening, makes it difficult to drain from the sinus. In some cases (10%) posterior to the first, main opening, there is a second, auxiliary opening.
Through the maxillary opening, air is exchanged in the sinus. Doctors have established that with a normally functioning hole, 90% of air is exchanged in the cavity for 5 minutes. The patency of the maxillary foramen is of great importance in the development of pathological processes in the sinus.
The inner wall in the upper-posterior part is in close contact with the cells of the ethmoid labyrinth, which in some cases protrude into the sinus.
The upper wall of the maxillary sinus is the lower wall of the orbit. This is a thin bone plate, in which sometimes there are dehiscences covered with a mucous membrane. In the thickness of this plate is the infraorbital canal, in which the nerve, artery and vein of the same name pass. The channel in the form of a roller is contoured on the lower, sinus surface of the plate. Inogra in the specified roller there are clefts and then the nerve and vessels passing in the canal are covered only by a thin mucous membrane, which should be taken into account when scraping the upper wall during maxillary sinusectomy.
The anterior, or facial, wall is the thickest, covered by the soft tissues of the cheek and accessible to palpation. In the center of the anterior wall there is a recess - the canine fossa, which serves as a guide when opening the mandibular sinus. This is where the bone is thinnest. At the upper edge of the canine fossa there is a hole through which the second branch comes to the surface. trigeminal nerve- infraorbital nerve. The posterior wall borders on the infratemporal and pterygopalatine fossae, in the latter there is a pterygoid venous plexus.
The lower wall of the maxillary sinus is the posterior part of the alveolar process of the upper jaw. The lower wall is in close contact with the holes of the first, second large molars and two small molars. In some cases, there is no bone tissue in the region of individual holes, and then the tops of the roots come into direct contact with the mucous membrane of the sinus floor. The lower wall of the maxillary sinus of medium size is at the level of the bottom of the nasal cavity, but is often located above or below the latter. According to studies, the bottom of the maxillary sinus in 42.8% of cases is below the lower nasal passage, in 39.3% - on the same level with it and in 17.9% - above it.
Due to the close contact of the lower wall of the maxillary sinus with the roots of the teeth of the upper jaw, inflammatory processes in the tips of the roots can cause inflammation of the maxillary sinus.
By the time the sinus is fully developed, four depressions, or bays, are distinguished in it: alveolar, zygomatic, palatine and frontal. Often on the lower wall there are bone protrusions in the form of ridges, which partially, and in some cases completely, divide the sinus into two chambers. The septa in the maxillary sinus may be either solid or with small openings. The formation of additional maxillary sinuses can also occur due to the ingrowth of one of the lattice cells. The capacity of these sinuses in adults ranges from 0.2-3.62 cm3.
Of course, the presence of partitions dividing the sinus into separate parts is of great practical importance, since thanks to them the disease can be unrecognized, and washing the sinus during puncture is difficult.
All anomalies of the maxillary sinuses can be detected on radiographs. X-ray anomalies are detected in 13.3% of patients.
The absorption capacity of the mucous membrane and the emigration of leukocytes are regarded as manifestations of the protective function of the membrane of the paranasal sinuses.
The blood supply to the paranasal sinuses is provided by branches of the internal and external carotid arteries, mainly through the ophthalmic, external and internal maxillary arteries. The maxillary sinus is fed mainly by the posterior superior alveolar artery and the anterior superior alveolar arteries - branches of the maxillary artery.
The outflow of blood from the paranasal sinuses is carried out through vessels that abundantly anastomose with each other, with the veins of the nose, face, orbit, cranial cavity, and cranial sinuses.
The venous system of the nose and paranasal sinuses is of great importance for the spread of infection.
The outflow of lymph from the paranasal sinuses occurs to the deep cervical and pharyngeal nodes. Through the lymphatic pathways, the infection can spread to the deep parts of the neck and mediastinum.
The innervation of the paranasal sinuses is carried out by the first and second branches of the trigeminal nerve and the fibers of the pterygopalatine ganglion.
In general, the maxillary sinus, like the other paranasal sinuses, protects the nerve structures of the orbit and anterior cranial fossa from breath-induced cooling and mechanical damage. In addition, the paranasal sinuses improve the respiratory function of the nose, serve to moisten the nasal mucosa and perform a resonator function.
Topic. The structure of the speech-motor sensory system
1. The structure of the peripheral part of the speech-motor sensory system.
1.1. The structure of the nose and nasal cavity.
1.2. The structure of the mouth and oral cavity.
1.3. The structure of the throat.
1.4. The structure of the larynx.
2. Conductive and cortical sections of the speech-motor sensory system. Brief description, meaning.
The structure of the peripheral part of the speech-motor sensory system.
The structure of the nose and nasal cavity
The nose consists of the external nose and the nasal cavity.
The external nose is formed by:
nasal bones,
nasal cartilage;
Bone processes of the palatine bone;
Processes of the maxillary bone.
Together, these structures make up the bone-cartilaginous skeleton. The nose also has soft tissues, which are located in the lateral sections and form the wings of the nose. At the bottom, they round off and form the nostrils. The front surface of the nose is lined with skin, the back surface is lined with mucous, which has a complex structure.
In the center of the nasal cavity is a septum that divides it in half. The nasal septum is a strong bone plate that normally has no holes. Sometimes there is a congenital curvature of the septum. If it interferes with full nasal breathing, then it is recommended surgical treatment. Each half of the nasal cavity has 4 walls:
1. Upper - it is formed by a lattice plate. The peculiarity of its structure is that it has numerous holes. Through them pass the threads of the olfactory nerve.
2. The lower wall is formed by the hard palate. The hard palate is also the upper wall of the oral cavity. It is formed by processes of the maxillary bones and palatine bones.
3. Inner wall - nasal septum.
4. The outer wall has a complex structure. On it in the horizontal direction there are 3 parallel bony protrusions, which in shape resemble half of a bivalve shell - they are called nasal conchas. There are 6 of them in total. Under the nasal conchas there are recesses, which are called the upper, middle, lower nasal passage.
The slit-like space between the nasal septum and the turbinates is called the common nasal passage. In front, the nasal cavity is covered by the external nose and has communication with air only through the nostrils. On the back wall of the nasal cavity there are 2 oval openings: choanae.
The entire nasal cavity is lined with mucous membranes. In the part of the mucous membrane that covers upper part nasal septum, upper and partly middle turbinate, branches of the olfactory nerve branch, ending in olfactory cells. This part of the nasal cavity is called the olfactory region. The rest of the nasal cavity is called the respiratory region.
The mucous membrane of the respiratory region is lined with ciliated epithelium. Under the layer of epithelium there are many glands that secrete mucus.
In the mucous membrane of the turbinates, especially the lower one, the so-called cavernous tissue, consisting of dilated venous plexuses, is laid. The walls of these plexuses contain a large number of smooth muscle fibers. When exposed to various stimuli (temperature, chemical), as well as mental factors, cavernous tissue that can quickly swell as a result of reflex expansion of the venous plexuses and filling them with blood. This swelling and causes sometimes sudden stuffing of the nose.
In the mucous membrane of the middle part of the nasal septum, approximately 1 cm posterior to the entrance to the nose, there is an area with a superficially located network of blood vessels. This area is called the bleeding zone of the nasal septum and is the most common source of nosebleeds.
Figure 1. The structure of the nasal septum and the lateral wall of the nasal cavity
The nasal cavity has a number of paranasal sinuses - sinuses. The sinuses are located in the surrounding bone nasal cavity. All paranasal sinuses are paired. In the frontal bones are the frontal sinuses; in the upper jaw - maxillary, or maxillary sinuses; in the sphenoid bone - sphenoid and in the ethmoid bone - ethmoid cells. The walls of the paranasal sinuses are lined with a thin mucous membrane, which is a continuation of the nasal mucosa. Therefore, an infection from the nasal cavity can pass to the sinuses, causing them to become inflamed (sinusitis).
In a newborn, the paranasal sinuses are in their infancy, and the frontal sinuses are absent. The ethmoid sinuses develop faster than others. The maxillary sinuses reach full development only by the end of the eruption of permanent teeth, and the frontal sinuses begin to form at the age of 4-6 years and complete development by the age of 20-25.
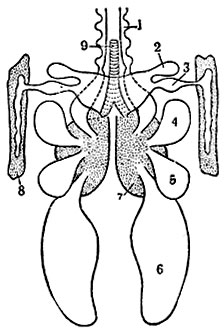
RESPIRATORY APPARATUS, a set of organs involved in gas exchange (see. Breath). Yes. can be divided into 3 sections: 1) the organs of the nasal cavity with the organ of smell; 2) larynx with vocal apparatus; 3) lungs - an organ of gas exchange. The pharynx is located between the nasal cavity and the larynx, and the trachea lies between the larynx and the lungs.
Organs of the nasal cavity (Fig. 1). The nasal cavity has inlets, nostrils, capable of several. expand (strongly in horses), and exit openings into the pharynx-choanae. The nasal cavity is divided by the nasal septum into right and left halves. In each half there are folds of the mucous membrane with thin bony leaves set into them. Of these folds, 2 large ones are called shells. The olfactory region lies in the posterior part of the nasal cavity, adjoining the bone lattice plate (lamina horisontalis), which has a large number of holes in the cavity of the cerebral skull, to the brain. The olfactory region is covered with a specific olfactory epithelium with a huge number of nerve sensitive cells. Each cell with one short, superficial, process perceives the sensation of smell, and with another, long, it transmits the perceived sensation to the brain. The rest of the nasal cavity is lined with ciliated epithelium, passing at the nostrils into the epithelium of the skin. The nasal cavity communicates with holes with several. adjacent additional air cavities - sinuses. The most extensive of them: 1) the maxillary sinus, or maxillary cave, located in the thickness of the upper jaw; 2) the frontal sinus, located in the thickness of the frontal bone.
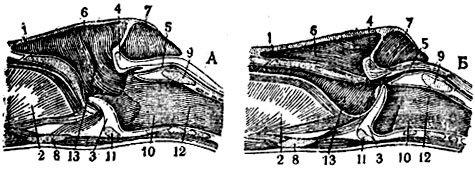
The larynx (Fig. 2) is located at the transition of the head to the neck. It represents an expanded part of the respiratory tract and consists of several. connected with each other cartilage, which make up its complex, mobile, connected into a single skeleton, supplied with muscles and lined inside with a mucous membrane. Three cartilages protruding forward (into the pharynx) - the epiglottis and a pair of arytenoid cartilages, dressed in a mucous membrane, play the role of valves that cover the entrance to the larynx from the pharynx during swallowing. Inside the larynx there are 2 folds of the mucous membrane with vocal cords and muscles. By the action of the musculature, these folds can tighten, narrowing the gap; increased inhalation movements cause them to oscillate and make a sound.
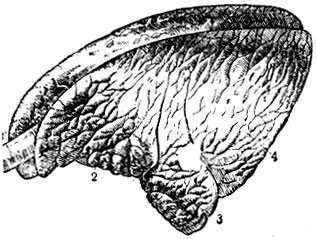
The trachea, or windpipe (Fig. 3, 1), is a wide hollow tube lying in the neck. It consists of interconnected cartilaginous rings and is lined with a mucous membrane with ciliated epithelium. By oscillating the cilia towards the larynx, the tube is cleared of contaminants that enter with the air. In the chest cavity, the trachea is divided into 2 (right and left) large bronchus (2 tubes similar in structure to the trachea), which enter the corresponding lung (right and left). Each bronchus, branching out in a tree-like manner and gradually losing its cartilaginous base, turns into a terminal bronchus (bronchiole), dividing into 2-3 alveolar passages with funnels at the ends. The wall of the alveolar passages and funnels consists of a single-layer squamous epithelium and a connective tissue membrane.
Lung (Fig. 3) - the main organ respiratory apparatus terrestrial vertebrates. There are two lungs, right and left. They are placed in the chest cavity, cover the heart and are built the same way. Lungs are lobulated; they have an anterior lobe (apex), a posterior lobe (base), and a middle lobe (cardiac).
The lung is arranged in such a way that atmospheric oxygen has the ability to approach the blood vessels over a fairly large area. A large bronchus entering the lung branches tree-like into smaller bronchi, which end in pulmonary lobules (Fig. 4), which are small areas lung tissue diam. OK. 1 cm. Inside the lobule, the bronchus is divided into the thinnest branches, dia. 0.5 m - terminal bronchi. The final bronchus is again divided into 2 respiratory bronchioles and, and each of them - into alveolar passages and funnels, passing into alveolar sacs. On the walls of the alveolar passages and sacs are protrusions (bubbles) - pulmonary alveoli.

From the heart to the lungs there is a large vessel - the pulmonary artery. Her used blood is relatively rich in carbon dioxide and poor in oxygen. This vessel, penetrating into the lungs, branches parallel to the branches of the bronchi and gives on the convex surfaces of the alveoli a dense network of the thinnest blood vessels - capillaries. The thinned walls of the alveoli and capillaries allow gases to diffuse; carbon dioxide goes into the air, and oxygen into the blood.
The chest cavity is lined inside with a thin shell - the parietal pleura (costal and diaphragmatic); the lungs are dressed in the same shell - the pulmonary pleura. Between the pulmonary and parietal pleura there is a narrow gap with a small amount of serous fluid, due to which the lobes of the lungs lie b. or m. freely in the chest cavity. Ventilation, i.e., the influx of fresh air into the alveoli and the outflow of used air, occurs due to the expansion and narrowing of the chest cavity.
Yes. in birds. The nasal cavity is very small, with 2 or 3 shells, without an ethmoid labyrinth. At the base of the larynx there is an annular cartilage, divided into 4 parts, and arytenoid cartilages. The epiglottis represents only a very slight transverse mucosal fold (without cartilage) at the entrance to the larynx. vocal folds birds do not, but at the border of the transition of the windpipe to the main bronchi there is a posterior (singing) larynx, which serves as a vocal apparatus. The lungs of birds (Fig. 5) lie tightly in the recesses of the upper part of the costal wall from the first rib to the location of the kidneys. Each main bronchus enters the lung, expands like an ampulla, loses its cartilaginous framework and, decreasing in diameter, stretches to the end of the lungs, where it passes into the abdominal air sacs. The branches in the lung communicate with each other by a system of tubes called parabronchi, from which the respiratory funnels with alveoli already diverge. There is a whole system of air sacs - cervical, clavicular, axillary, thoracic (anterior and posterior) and abdominal (the largest); many of them communicate with bone cavities.
The air sacs are assigned a variety of meanings. They serve to facilitate flight, to move the center of gravity with different filling, to regulate the temperature (due to the absence of sweat glands in skin). They are also probably reserve air reservoirs for maintaining gas exchange in the absence of respiratory movements, as well as air reservoirs for singing.
D.'s diseases and. cm. Rhinitis, Laryngitis, Laringo-tracheitis of birds, Wheezing choking, Bronchitis, Contagious catarrh of the upper respiratory tract of horses, Pneumonia, Contagious pleuropneumonia of horses, General inflammation of the lungs of cattle, Emphysema, Pleurisy.
A. Klimov
Literature: Autocrats D., Course of anatomy of poultry, M.-L., 1928; his, Anatomy of domestic animals, M., 1949; Viktorov K., Physiology of domestic animals, 4th ed., M., 1948; Klimov A., Anatomy of domestic animals, vol. I, 2nd ed., M., 1941; his own. Anatomy and physiology of farm animals, 5th ed., M., 1946.
Sources:
- Agricultural Encyclopedia. T. 1 (A - E) / Ed. collegium: P. P. Lobanov (chief editor) [and others]. Third edition, revised - M., State publishing house of agricultural literature, 1949, p. 620
Clinical anatomy of the nose
The nose is the initial part of the upper respiratory tract and is divided into three sections: - External nose. - Nasal cavity. - Paranasal sinuses. External nose The external nose is a bone-cartilaginous pyramid covered with skin. The following elements of the external nose are distinguished: root, back, slopes, wings and tip. Its walls are formed by the following tissues: bone, cartilage and skin. 1. The bone part of the skeleton consists of the following elements: paired nasal bones; frontal processes of the upper jaw; nasal process of the frontal bone. 2. Cartilages of the external nose are paired: triangular; wing; additional. 3. The skin covering the nose has the following features: an abundance of sebaceous glands, mainly in the lower third of the external nose; a large number of hairs on the eve of the nose, performing protective function; an abundance of blood vessels that anastomose with each other. The blood supply to the external nose is carried out as follows: arterial blood comes from the system of external and internal carotid arteries; venous outflow occurs through the facial vein into the ophthalmic vein, then into the cavernous sinus located in the cranial cavity and further into the internal jugular vein. This structure of the venous system is of great clinical importance, as it can contribute to the development of orbital and intracranial complications. Lymph outflow from the tissues of the external nose is carried out mainly in the submandibular The lymph nodes. Innervation is provided by branches facial nerve, the first and second branches of the trigeminal nerve. Nasal cavity The nasal cavity is the space between the anterior cranial fossa and the oral cavity. The nasal cavity is divided by a septum into right and left halves and has anterior openings - nostrils and posterior - choanae leading to the nasopharynx. Each half of the nose has four walls. The medial wall, or nasal septum, is formed by: a quadrangular cartilage in the anterior section; perpendicular plate of the ethmoid bone in the upper section; vomer in the lower back section. The upper wall consists of a perforated plate of the ethmoid bone, through which the branches of the olfactory nerve and vessels pass. The lower wall, or the bottom of the nasal cavity, is formed by: the alveolar process of the upper jaw; palatine process of the upper jaw; horizontal plate of the palatine bone. The lateral wall, which has the greatest clinical significance, is the most complex in structure. It is formed by the following bones: nasal, lacrimal, ethmoid, main and palatine. On the inner surface of the lateral wall there are three bony protrusions - nasal conchas. The superior and middle turbinates are processes of the ethmoid bone, while the inferior is an independent bone. Under the shells are the corresponding nasal passages - upper, middle and lower. The space between the nasal septum and the edges of the turbinates forms a common nasal passage. In children early age the inferior nasal concha fits snugly to the bottom of the nasal cavity, which leads to a complete shutdown of nasal breathing even with a slight inflammation of the mucosa. Anatomical formations located in the nasal passages are of great clinical importance: the outlet of the nasolacrimal canal opens into the lower nasal passage, a delay in its opening leads to disruption of the outflow of tears, cystic dilation of the canal and narrowing of the nasal passages in newborns; the maxillary sinus opens into the middle nasal passage, in the anterior upper section - the canal of the frontal sinus, in the middle part of the passage - the anterior and middle cells of the ethmoid bone; the sphenoid sinus and the posterior cells of the ethmoid labyrinth open into the upper nasal passage. The nasal cavity can be divided into three regions: vestibule, respiratory and olfactory. The vestibule is limited by the wings of the nose, its edge is lined with a strip of skin 4-5 mm, equipped with a large number of hairs that perform a protective function, but also create conditions for the occurrence of boils and sycosis. The respiratory region occupies the space from the bottom of the nasal cavity to the lower edge of the middle turbinate and is lined with mucosa with a cylindrical ciliated epithelium. It contains a large number of goblet cells that secrete mucus, and branched alveolar glands that produce a serous secret. The movement of the cilia of the ciliated epithelium is directed towards the choanae. Under the mucous membrane of the turbinates there is a tissue consisting of a plexus of vessels and resembling cavernous tissue. The latter contributes to the instantaneous swelling of the mucosa and narrowing of the nasal passages under the influence of physical, chemical and psychogenic stimuli. The olfactory region is located in the upper-posterior part of the nasal cavity, its boundary is the lower edge of the middle turbinate. This zone is lined with olfactory epithelium containing olfactory spindle cells, supporting cells and glands that produce a special secret to dissolve organic substances. Blood supply to the nasal cavity: branches of the external carotid artery provide lower posterior sections; branches of the internal carotid artery supply the upper anterior parts of the nasal cavity; venous vessels accompany arteries. Through the venous plexuses, there is a connection with the veins of the skull, orbit, pharynx, which creates the possibility of the spread of infection and the development of complications. In the anterior third of the nasal septum there is a section of the superficial capillary network, called the bleeding zone, or the Kisselbach zone. Lymph drainage is carried out to the submandibular and deep cervical lymph nodes, in addition, it has a connection with the cranial cavity along the olfactory pathways. Innervation is divided into the following types: sensitive, which is provided by the first and second branches of the trigeminal nerve; olfactory, represented by the olfactory epithelium, the olfactory bulb and the central part of the olfactory analyzer; secretory, which is provided by the fibers of the sympathetic and parasympathetic nervous system. And now more clearly, in detail and abstrusely.
The basis of the cartilaginous section of the external nose is the lateral cartilage, the upper edge of which borders on the nasal bone of the same side and partially on the frontal process of the upper jaw. The upper faces of the lateral cartilages constitute a continuation of the back of the nose, adjoining in this section to the cartilaginous part of the upper parts of the nasal septum. The lower face of the lateral cartilage borders on the large cartilage of the wing, which is also paired. The large cartilage of the wing has a medial and lateral crura. Connecting in the middle, the medial legs form the tip of the nose, and the lower sections of the lateral legs are the edge of the nasal openings (nostrils). Sesamoid cartilages of various shapes and sizes can be located between the lateral and greater cartilages of the wing of the nose in the thickness of the connective tissue. The alar of the nose, in addition to the large cartilage, includes connective tissue formations, from which the posterior inferior parts of the nasal openings are formed. The inner sections of the nostrils are formed by the movable part of the nasal septum. The outer nose is covered with the same skin as the face. The external nose has muscles that are designed to compress the nasal openings and pull down the wings of the nose. The blood supply to the external nose is provided by the ophthalmic artery (a. ophtalmis), dorsal nasal (a. dorsalis nasi) and facial (a. facialis) arteries. Venous outflow is carried out through the facial, angular and partially ophthalmic veins, which in some cases contributes to the spread of infection when inflammatory diseases external nose to the sinuses of the hard meninges. Lymphatic drainage from the external nose occurs in the submandibular and upper parotid lymph nodes. The motor innervation of the external nose is provided by the facial nerve, the sensory innervation is provided by the trigeminal (I and II branches). The anatomy of the nasal cavity is more complex. The nasal cavity is located between the anterior cranial fossa (above), the orbits (laterally) and the oral cavity (below). From the front, the nasal cavity communicates with the external environment through the nostrils, from behind, with the help of the choanae, it communicates with the nasopharyngeal region. There are four walls of the nasal cavity: lateral (lateral), internal (medial), upper and lower. The most complex structure is the side wall of the nose, formed by several bones and carrying the nasal conchas. Of the bone formations, it consists of the nasal bones, the upper jaw, the lacrimal bone, the ethmoid bone, the inferior nasal concha, the vertical plate of the palatine bone and the pterygoid process. sphenoid bone. On the side wall there are three longitudinal protrusions formed by shells. The largest is the inferior turbinate, it is an independent bone, the middle and superior shells are outgrowths of the ethmoid bone. The lower wall of the nasal cavity (the bottom of the nasal cavity) is actually a hard palate, it is formed by the palatine process of the upper jaw (in the anterior sections) and the horizontal plate of the palatine bone. At the anterior end of the bottom of the nose there is a canal that serves to pass the nasopalatine nerve (n. Nasopalatinus) from the nasal cavity into the oral cavity. The horizontal plate of the palatine bone limits the lower sections of the choanae. The inner (medial) wall of the nasal cavity is the nasal septum (Fig. 2). In the lower and posterior sections, it is represented by bone formations (the nasal crest of the palatine process of the upper jaw, the perpendicular plate of the ethmoid bone and an independent bone - the vomer). In the anterior sections to these bone formations the quadrangular cartilage of the nasal septum (cartilage septi nasi) adjoins, the upper edge of which forms the anterior part of the back of the nose. The posterior edge of the vomer limits the choanae medially. In the anteroinferior section, the cartilage of the nasal septum is adjacent to the medial processes of the large cartilage of the alar of the nose, which, together with the skin part of the nasal septum, constitute its movable part.
The upper wall of the nasal cavity (roof) in the anterior sections is formed by the nasal bones, the frontal processes of the upper jaw, and a partially perpendicular plate of the ethmoid bone. In the middle sections, the upper wall is formed by the ethmoid (perforated) plate (lamina cribrosa) of the ethmoid bone, in the posterior - by the sphenoid bone (anterior wall of the sphenoid sinus). The sphenoid bone forms the superior wall of the choana. The cribriform plate is pierced by a large number (25-30) holes through which the branches of the anterior ethmoidal nerve and the vein that accompanies the anterior ethmoid artery and connects the nasal cavity with the anterior cranial fossa pass. The space between the nasal septum and the turbinates is called the common nasal passage. In the lateral parts of the nasal cavity, respectively, there are three nasal passages. The lower nasal passage (meatus nasi inferior) is limited from above by the inferior nasal concha, from below - by the bottom of the nasal cavity. In the anterior third of the lower nasal passage, at a distance of 10 mm from the anterior end of the shell, there is an opening of the nasolacrimal canal. The lateral wall of the lower nasal passage in the lower sections is thick (has a spongy structure), closer to the place of attachment of the lower nasal concha, it becomes significantly thinner, and therefore the puncture of the maxillary sinus is performed precisely in this area: 2 cm away from the anterior end of the lower one.
The middle nasal passage (meatus nasi medius) is located between the lower and middle nasal conchas. Its lateral wall is represented not only bone tissue , but also a duplication of the mucous membrane, which is called "fontanels" (fontanelles). If the middle turbinate is partially removed, then the semilunar cleft (hiatus semilunaris) will open, in the anteroinferior sections it is limited by the bone plate (uncinate process), in the posterior superior regions by the bone vesicle (bulla etmoidalis). In the anterior sections of the semilunar fissure, the mouth of the frontal sinus opens, in the middle sections - the anterior and middle cells of the ethmoid sinuses, and in the posterior sections there is a depression formed by a duplication of the mucous membrane and called a funnel (infundibulum), which ends with a hole leading to the maxillary sinus. The superior nasal passage (meatus nasi superior) is located between the superior and middle nasal conchas. The posterior cells of the ethmoid bone open into it. The sphenoid sinus opens into the sphenoid-ethmoid recess (recessus spheno-ethmoidalis). The nasal cavity is lined with a mucous membrane that covers all the bone sections of the walls, and therefore the contours of the bone section are preserved. The exception is the vestibule of the nasal cavity, which is covered with skin and has hairs (vibrissae). In this area, the epithelium remains stratified squamous, as in the area of the external nose. The mucous membrane of the nasal cavity is covered with multi-row cylindrical ciliated epithelium. Depending on the structural features of the nasal mucosa, the respiratory and olfactory sections are distinguished. The respiratory section occupies the area from the bottom of the nasal cavity to the middle of the middle turbinate. Above this limit, the ciliated columnar epithelium is replaced by a specific olfactory epithelium. The respiratory section of the nasal cavity is characterized by a large thickness of the mucous membrane. Its subepithelial section contains numerous alveolar-tubular glands, which, according to the nature of the secret, are divided into mucous, serous, and mixed. The respiratory part of the mucous membrane is characterized by the presence in its thickness of cavernous plexuses - varicose venous sheaths with a muscular wall, due to which they can contract in volume. Cavernous plexuses (cavernous bodies) provide regulation of the temperature of the air passing through the nasal cavity. Cavernous tissue is contained in the thickness of the mucous membrane of the inferior turbinates, located along the lower edge of the middle turbinate, in the posterior sections of the middle and superior turbinates. In the olfactory region, in addition to the specific olfactory epithelium, there are supporting cells that are cylindrical, but lack cilia. The glands present in this part of the nasal cavity secrete a more liquid secret than the glands located in the respiratory part. The blood supply to the nasal cavity is carried out from the system of external (a. carotis externa) and internal (a. carotis interim) carotid arteries. The main palatine artery (a. sphenopalatina) originates from the first artery; passing through the main palatine opening (foramen sphenopalatinum) into the nasal cavity, it gives off two branches - the posterior nasal lateral and septal arteries (aa. nasales posteriores laterales et septi), which provide blood supply to the posterior sections of the nasal cavity, both lateral and medial walls. The ophthalmic artery originates from the internal carotid artery, from which the branches of the anterior and posterior ethmoidal arteries (aa. ethmoidales anterior et posterior) depart. The anterior ethmoidal arteries pass into the nose through the cribriform plate, the posterior ones through the posterior ethmoidal foramen (foramen ethmoidale post.). They provide nutrition to the area of the ethmoidal labyrinth and the anterior parts of the nasal cavity. The outflow of blood is carried out through the anterior facial and ophthalmic veins. Features of the outflow of blood often cause the development of ophthalmic and intracranial rhinogenic complications. In the nasal cavity, especially pronounced venous plexuses are found in the anterior sections of the nasal septum (locus Kilsselbachii). Lymphatic vessels form two networks - superficial and deep. The olfactory and respiratory regions, despite their relative independence, have anastomoses. Lymph outflow occurs in the same lymph nodes: from the anterior parts of the nose to the submandibular, from the posterior to the deep cervical. Sensitive innervation of the nasal cavity is provided by the first and second branches of the trigeminal nerve. The anterior nasal cavity is innervated by the first branch of the trigeminal nerve (anterior ethmoid nerve - n. ethmoidalis anterior-branch of the nasociliary nerve - n. nasociliaris). The nasociliary nerve from the nasal cavity penetrates through the nasociliary foramen (foramen nasociliaris) into the cranial cavity, and from there through the cribriform plate into the nasal cavity, where it branches in the region of the nasal septum and the anterior sections of the lateral wall of the nose. The external nasal branch (ramus nasalis ext.) between the nasal bone and the lateral cartilage extends to the back of the nose, innervating the skin of the external nose. The posterior parts of the nasal cavity are innervated by the second branch of the trigeminal nerve, which enters the nasal cavity through the posterior ethmoid foramen and branches in the mucous membrane of the posterior cells of the ethmoid bone and the sinus of the sphenoid bone. The nodal branches and the infraorbital nerve depart from the second branch of the trigeminal nerve. The nodal branches are part of the pterygopalatine node, however, most of them pass directly into the nasal cavity and innervates the posterior superior part of the lateral wall of the nasal cavity in the region of the middle and superior turbinates, the posterior cells of the ethmoid bone and the sinus of the sphenoid bone in the form of rr. nasales. Along the nasal septum in the direction from back to front there is a large branch - the nasopalatine nerve (n. Nasopalatinus). In the anterior parts of the nose, it penetrates through the incisive canal into the mucous membrane of the hard palate, where it anastomoses with the nasal branches of the alveolar and palatine nerves. Secretory and vascular innervation is carried out from the superior cervical sympathetic ganglion, the postganglionic fibers of which penetrate the nasal cavity as part of the second branch of the trigeminal nerve; parasympathetic innervation is carried out through the pterygopalatine ganglion (gang. pterigopalatinum) due to the nerve of the pterygoid canal. Last formed sympathetic nerve, extending from the upper cervical sympathetic node, and the parasympathetic nerve, originating from the geniculate node of the facial nerve. Specific olfactory innervation is carried out by the olfactory nerve (n. olfactorius). Sensory bipolar cells of the olfactory nerve (I neuron) are located in the olfactory region of the nasal cavity. The olfactory filaments (filae olfactoriae) extending from these cells penetrate the cranial cavity through the cribriform plate, where, when combined, they form an olfactory bulb (bulbus olfactorius), enclosed in a vagina formed by the dura mater. The pulpy fibers of the sensory cells of the olfactory bulb form the olfactory tract (tractus olfactorius - neuron II). Further, the olfactory pathways go to the olfactory triangle and end in the cortical centers (gyrus hippocampi, gyrus dentatus, sulcus olfactorius).
Clinical anatomy of the paranasal sinuses
The paranasal sinuses are air cavities located around the nasal cavity and communicating with it through excretory openings or ducts. There are four pairs of sinuses: maxillary, frontal, ethmoid labyrinth and sphenoid (basic). The clinic distinguishes between the anterior sinuses (maxillary, frontal and anterior and middle ethmoid) and posterior (posterior ethmoid cells and sphenoid). Such a subdivision is convenient from a diagnostic standpoint, since the anterior sinuses open into the middle nasal passage, and the posterior sinuses open into the upper nasal passage. The maxillary sinus, (aka maxillary sinus) located in the body of the maxillary bone, is an irregularly shaped pyramid ranging in size from 15 to 20 cm3. The anterior or facial wall of the sinus has a depression called the canine fossa. In this area, the sinus is usually opened. The medial wall is the lateral wall of the nasal cavity and contains a natural outlet in the region of the middle nasal passage. It is located almost under the roof of the sinus, which makes it difficult for the outflow of contents and contributes to the development of congestive inflammatory processes. The upper wall of the sinus simultaneously represents the lower wall of the orbit. It is quite thin, often has bone clefts, which contributes to the development of intraorbital complications. The lower wall is formed by the alveolar process of the maxilla and usually occupies the space from the second premolar to the second molar. The low position of the bottom of the sinus contributes to the proximity of the roots of the teeth to the sinus cavity. In some cases, the tops of the roots of the teeth stand in the lumen of the sinus and are only covered by the mucous membrane, which can contribute to the development of odontogenic infection of the sinus, the ingress of filling material into the sinus cavity, or the formation of a persistent perforation during tooth extraction. The posterior wall of the sinus is thick, bordering the cells of the ethmoid labyrinth and the sphenoid sinus. The frontal sinus is located in the thickness of the frontal bone and has four walls: the lower orbital - the thinnest, the anterior - the thickest up to 5-8 mm, the posterior, separating the sinus from the anterior cranial fossa, and the internal - the septum. The frontal sinus communicates with the nasal cavity through a thin tortuous canal that opens into the anterior middle meatus. The size of the sinus ranges from 3 to 5 cm3, and in 10-15% of cases it may be absent. The ethmoid labyrinth is located between the orbit and the nasal cavity and consists of 5-20 air cells, each of which has its own outlet openings into the nasal cavity. There are three groups of cells: anterior and middle, opening into the middle nasal passage, and posterior, opening into the upper nasal passage. The sphenoid, or main, sinus is located in the body of the sphenoid bone, divided by a septum into two halves, which have an independent exit to the region of the upper nasal passage. Near the sphenoid sinus are the cavernous sinus, carotid artery, optic chiasm, pituitary gland. As a result, the inflammatory process of the sphenoid sinus is a serious danger. The blood supply to the paranasal sinuses occurs due to the branches of the external and internal carotid arteries. The veins of the maxillary sinus form numerous anastomoses with the veins of the orbit, nose, sinuses of the dura mater. Lymphatic vessels are closely connected with the vessels of the nasal cavity, vessels of the teeth, pharyngeal and deep cervical lymph nodes. Innervation is carried out by the first and second branches of the trigeminal nerve. Features of the structure of the paranasal sinuses in childhood Newborns have only two sinuses: the maxillary sinus and the ethmoid labyrinth. The maxillary sinus is a fold of mucous about 1 cm long at the inner corner of the orbit, laterally, under the lower wall of the orbit, there are two rows of rudiments of milk and permanent teeth. By the end of the first year of life, the sinus acquires a rounded shape. By the age of 6-7, the teeth gradually take their position, and the sinus becomes multifaceted. In early childhood, the canine is closest to the sinus; at 6 years old, two premolars and a molar are located. By the age of 12, the volume of the sinus increases and the topography approaches the norm of an adult. The cells of the ethmoid labyrinth in newborns are in their infancy and fully develop by the age of 14-16. The frontal and sphenoid sinuses are absent in newborns and begin to form from 3-4 years of age. The frontal sinuses develop from the anterior cells of the ethmoid labyrinth and by the age of 6 have a volume of about 1 cm3. The sphenoid sinuses are formed from the cells of the ethmoid labyrinth located in the body of the sphenoid bone. The final development of the sinuses ends by 25-30 years.
